Atrial fibrillation (Afib) is a common cardiac arrhythmia characterized by irregular and often rapid heartbeats. It can lead to various complications, including stroke, heart failure, and other heart-related problems. Understanding the causes of Afib is crucial for its prevention and management. One question that arises is whether physical trauma, such as a fall, can cause Afib. This article explores the potential connection between falls and Afib, delving into the mechanisms, risk factors, and implications for patient care.
What Is Atrial Fibrillation?
Atrial fibrillation occurs when the electrical signals in the atria (the upper chambers of the heart) become disorganized, leading to an irregular and often rapid heart rate. This disruption in the heart’s electrical system can result in poor blood flow, as the atria are unable to effectively contract and move blood into the ventricles (the lower chambers of the heart). The main types of Afib are:
Paroxysmal Afib: Episodes that come and go, usually lasting less than 24 hours but can persist for up to a week.
Persistent Afib: Episodes that last more than a week and may require medical intervention to terminate.
Permanent Afib: Continuous and ongoing episodes that cannot be restored to normal rhythm.
SEE ALSO: Normal Sinus Rhythm Vs Sinus Arrhythmia: What’s The Different
Common Causes And Risk Factors of Atrial Fibrillation
Several factors contribute to the development of Afib, including:
Age: The risk of Afib increases with age, particularly in individuals over 60.
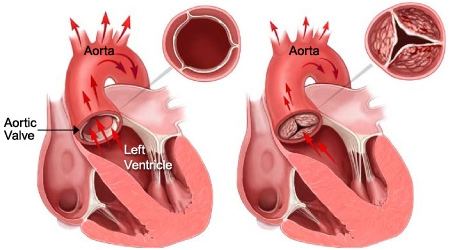
Heart disease: Conditions like hypertension, coronary artery disease, heart failure, and valvular heart disease are significant risk factors.
Lifestyle factors: Obesity, excessive alcohol consumption, smoking, and sedentary lifestyle.
Medical conditions: Thyroid disorders, sleep apnea, and diabetes.
Genetics: A family history of Afib can increase the likelihood of developing the condition.
Can A Fall Cause Atrial Fibrillation?
The relationship between physical trauma and the onset of Afib is complex and multifaceted. While a fall itself may not directly cause Afib, several mechanisms and circumstances associated with a fall can potentially trigger the condition.
Physical Trauma And Stress Response
A fall can result in significant physical trauma, leading to pain, injury, and a physiological stress response. This stress response involves the release of stress hormones such as adrenaline and cortisol, which can affect the heart’s electrical activity. The heightened sympathetic nervous system activity may increase the likelihood of arrhythmias, including Afib.
Inflammation And Injury
Injury from a fall can lead to localized inflammation, which can have systemic effects. Inflammation is known to play a role in the development of Afib. Studies have shown that elevated levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6), are associated with an increased risk of Afib.
Therefore, the inflammation resulting from a fall-related injury could contribute to the onset of Afib.
Autonomic Nervous System Imbalance
The autonomic nervous system, which regulates involuntary bodily functions, plays a crucial role in maintaining heart rhythm. A fall can disrupt the balance between the sympathetic (fight or flight) and parasympathetic (rest and digest) branches of the autonomic nervous system. This imbalance can predispose individuals to arrhythmias, including Afib.
Pre-existing Conditions
Individuals with pre-existing conditions such as hypertension, heart disease, or diabetes are already at an increased risk of Afib. A fall can exacerbate these conditions or lead to complications that may trigger Afib. For instance, a fall resulting in a head injury or fracture can cause additional stress on the cardiovascular system, increasing the likelihood of an arrhythmic event.
Psychological Stress And Anxiety
Falls, particularly in older adults, can lead to significant psychological stress and anxiety. The fear of falling again, coupled with the trauma of the initial fall, can elevate stress levels. Chronic stress and anxiety are known to increase the risk of Afib by affecting the heart’s electrical stability and promoting an inflammatory response.
Clinical Evidence And Case Studies
Research on the direct link between falls and Afib is limited, but some studies and case reports provide insights into the potential connection.
Case Report 1: Fall-Induced Afib in an Elderly Patient
A case study reported an 80-year-old patient who developed Afib following a fall. The patient had a history of hypertension and coronary artery disease. The fall resulted in a hip fracture, leading to significant pain and stress. Within 24 hours of the fall, the patient experienced palpitations and was diagnosed with Afib. The study suggested that the stress and inflammation from the injury likely contributed to the onset of Afib.
Study 1: Trauma and Cardiac Arrhythmias
A study examining the incidence of cardiac arrhythmias intrauma patients found that a significant proportion of patients developed arrhythmias, including Afib, following traumatic injuries. The study highlighted that the physiological stress response and inflammation associated with trauma could precipitate arrhythmic events.
Implications for Patient Care
Understanding the potential link between falls and Afib has important implications for patient care, particularly in the elderly population who are more prone to both falls and Afib.
Fall Prevention
Preventing falls is crucial in reducing the risk of fall-related complications, including Afib. Strategies for fall prevention include:
Home safety modifications: Removing tripping hazards, installing grab bars, and ensuring adequate lighting.
Physical therapy: Improving strength, balance, and coordination through targeted exercises.
Medication management: Reviewing medications that may increase the risk of falls, such as sedatives or blood pressure medications.
Monitoring And Early Detection
For individuals who have experienced a fall, particularly those with pre-existing cardiovascular conditions, close monitoring for signs of Afib is essential. Early detection and timely intervention can prevent complications and improve outcomes.
Healthcare providers should consider the following:
Electrocardiogram (ECG): Conducting an ECG to check for arrhythmias in patients who have experienced a fall.
Holter monitoring: Using a Holter monitor to detect intermittent episodes of Afib in patients with a history of falls and cardiovascular risk factors.
Stress and Anxiety Management
Addressing the psychological impact of falls is also important.
Providing support and resources to manage stress and anxiety can help reduce the risk of Afib. Interventions may include:
Counseling: Offering psychological counseling to address fear and anxiety related to falls.
Relaxation techniques: Teaching relaxation techniques such as deep breathing, meditation, and mindfulness.
Conclusion
While a fall itself may not be a direct cause of atrial fibrillation, the associated physical trauma, stress response, inflammation, autonomic nervous system imbalance, and exacerbation of pre-existing conditions can contribute to the onset of Afib. Understanding these mechanisms highlights the importance of fall prevention, monitoring for arrhythmias in fall-prone individuals, and managing stress and anxiety following a fall. By addressing these factors, healthcare providers can better prevent and manage Afib in patients at risk.