Endocarditis and myocarditis are both serious conditions affecting the heart, but they differ significantly in their origins, manifestations, and treatments. Understanding these differences is crucial for accurate diagnosis and appropriate management of these cardiac diseases. This article will explore the definitions, causes, symptoms, diagnostic methods, treatments, and prognoses of endocarditis and myocarditis, providing a comprehensive overview of their distinctions.
Definitions
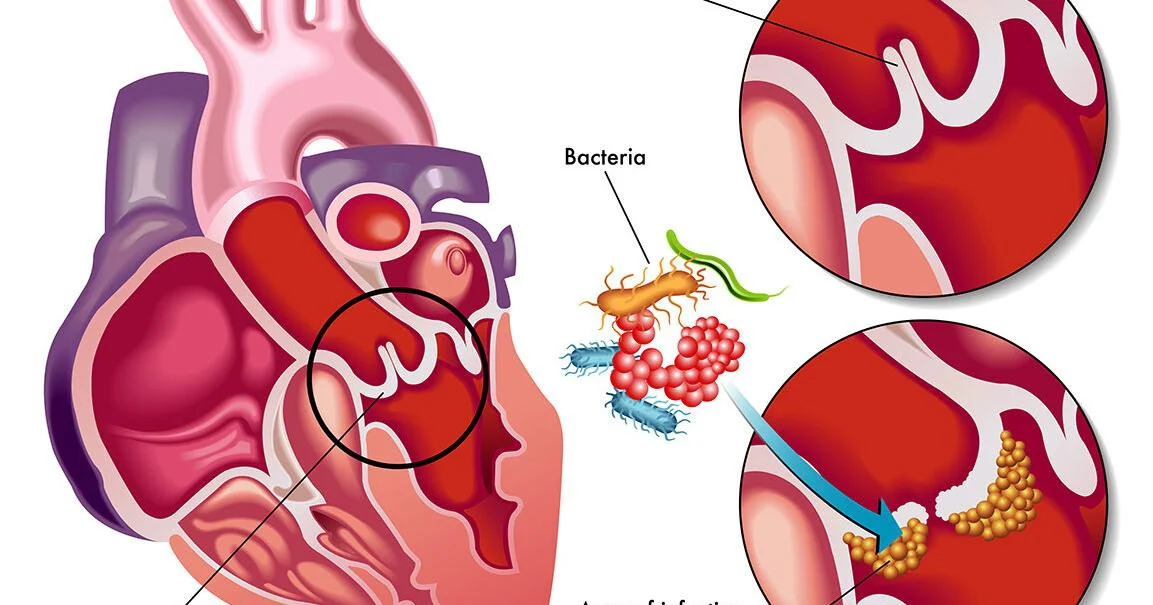
Endocarditis is the inflammation of the inner lining of the heart chambers and valves, known as the endocardium. This condition is typically caused by bacterial infection but can also result from fungal infections or other microorganisms. The inflammation can lead to the formation of vegetations—clusters of microorganisms and cellular debris—on the heart valves, which can cause severe complications if not treated promptly.
Myocarditis, on the other hand, is the inflammation of the heart muscle itself, known as the myocardium. This condition can be caused by viral infections, autoimmune diseases, or exposure to certain toxins. Myocarditis can impair the heart’s ability to pump blood effectively, potentially leading to heart failure or sudden cardiac death.
SEE ALSO: 8 Symptoms of COVID-19 Myocarditis
Endocarditis Vs Myocarditis: What Is The Difference
1. Causes
Endocarditis
The primary cause of endocarditis is an infection by bacteria, most commonly:
Staphylococcus aureus: This bacterium is responsible for both community-acquired and healthcare-associated infections.
Streptococcus viridans: Commonly found in the mouth, this bacterium can enter the bloodstream during dental procedures and cause endocarditis.
Enterococcus: Often originating from the gastrointestinal tract, these bacteria can cause endocarditis, particularly in older adults or those with underlying health conditions.
Other less common causes include fungal infections, such as those caused by Candida species, and other microorganisms.
Myocarditis
Myocarditis is primarily caused by viral infections. The most common viruses associated with myocarditis include:
Coxsackievirus: A group of enteroviruses that can cause inflammation of the myocardium.
Adenovirus: A common cause of respiratory infections that can also affect the heart.
Parvovirus B19: Known for causing fifth disease in children, this virus can also infect the heart muscle.
In addition to viral infections, myocarditis can result from:
Autoimmune diseases: Conditions such as lupus or rheumatoid arthritis can cause the immune system to attack the heart muscle.
Toxins: Exposure to certain chemicals, drugs, or alcohol can lead to myocarditis.
Bacterial infections: Although less common than viral causes, bacteria such as Borrelia burgdorferi (the causative agent of Lyme disease) can cause myocarditis.
2. Symptoms
Endocarditis
The symptoms of endocarditis can vary widely depending on the severity of the infection and the presence of underlying health conditions. Common symptoms include:
Fever and chills: Often the first signs of infection.
Heart murmurs: New or changed heart murmurs can indicate valve damage.
Fatigue: Persistent tiredness and weakness.
Aching joints and muscles: Generalized pain in muscles and joints.
Night sweats: Profuse sweating during sleep.
Shortness of breath: Difficulty breathing, especially with activity.
Swelling: Edema in the legs, feet, or abdomen.
Petechiae: Small, red or purple spots on the skin or inside the mouth.
Myocarditis
The symptoms of myocarditis can range from mild to severe and may include:
Chest pain: A sharp or stabbing pain in the chest.
Fatigue: Extreme tiredness and weakness.
Shortness of breath: Especially after exertion or while lying down.
Heart palpitations: Rapid or irregular heartbeats.
Swelling: Edema in the legs, ankles, and feet.
Flu-like symptoms: Fever, sore throat, and body aches.
In severe cases, myocarditis can lead to symptoms of heart failure, such as difficulty breathing, severe fatigue, and fluid retention.
3. Diagnostic Methods
Endocarditis
Diagnosing endocarditis involves a combination of clinical evaluation, laboratory tests, and imaging studies:
Blood cultures: Multiple blood samples are taken to identify the presence of bacteria or fungi in the bloodstream.
Echocardiography: This imaging test uses ultrasound to create pictures of the heart and can detect vegetations on the heart valves.
Electrocardiogram (ECG): This test measures the electrical activity of the heart and can identify abnormalities that may suggest endocarditis.
Chest X-ray: Used to check for fluid in the lungs or other complications.
Myocarditis
The diagnosis of myocarditis can be more challenging and typically involves:
Blood tests: To check for markers of inflammation and cardiac enzymes that indicate heart muscle damage.
Electrocardiogram (ECG): To detect electrical abnormalities in the heart.
Echocardiography: To assess heart function and check for inflammation or structural changes.
Cardiac MRI: This imaging test provides detailed pictures of the heart and can identify areas of inflammation.
Endomyocardial biopsy: A procedure where a small sample of heart tissue is taken for microscopic examination to confirm myocarditis.
4. Treatments
Endocarditis
The treatment of endocarditis depends on the causative organism and the severity of the condition:
Antibiotics: Long-term intravenous antibiotics are the primary treatment for bacterial endocarditis. The choice of antibiotics depends on the specific bacteria identified.
Antifungal medications: Used for fungal endocarditis.
Surgery: In severe cases, surgery may be required to repair or replace damaged heart valves or to remove infected tissue.
Myocarditis
The treatment of myocarditis focuses on managing symptoms and addressing the underlying cause:
Antiviral medications: Used if a specific virus is identified.
Immunosuppressive drugs: In cases of autoimmune myocarditis, medications that suppress the immune system may be used.
Heart medications: To reduce the workload on the heart and improve symptoms, such as beta-blockers, ACE inhibitors, and diuretics.
Rest and supportive care: Patients are often advised to rest and avoid strenuous activities to allow the heart to heal.
Mechanical support: In severe cases, devices like ventricular assist devices (VADs) may be used to support heart function.
5. Prognosis
Endocarditis
The prognosis for endocarditis depends on several factors, including the type of microorganism causing the infection, the speed of diagnosis and treatment, and the presence of any complications. With prompt and appropriate treatment, many patients recover fully, but untreated endocarditis can be fatal.
Myocarditis
The prognosis for myocarditis varies widely. Some individuals recover completely with appropriate treatment, while others may develop chronic heart problems or heart failure. Severe myocarditis can lead to life-threatening complications, including sudden cardiac death.
Conclusion
Endocarditis and myocarditis are both serious conditions that affect the heart, but they differ in their causes, symptoms, diagnostic methods, treatments, and prognoses. Endocarditis primarily involves an infection of the heart’s inner lining and valves, often caused by bacteria, while myocarditis involves inflammation of the heart muscle itself, usually due to viral infections. Understanding these differences is crucial for healthcare providers to make accurate diagnoses and provide effective treatments, ultimately improving patient outcomes.