A pacemaker is a small, battery-operated device implanted in the chest to help control heartbeats. It’s used for people with heart rhythm disorders (arrhythmias), where the heart may beat too slowly, too quickly, or irregularly. When functioning correctly, a pacemaker sends electrical impulses to stimulate the heart to beat at a normal rate. However, there are scenarios where a pacemaker may stop working or fail. Understanding the potential consequences and actions to take is crucial for individuals who rely on these life-saving devices.
How A Pacemaker Works
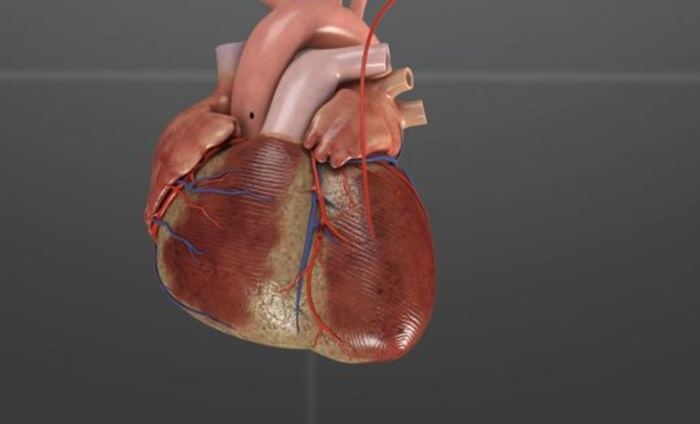
Before delving into what happens when a pacemaker stops, it’s essential to understand how it operates. A pacemaker consists of a pulse generator, which houses the battery and the electrical circuitry, and one or more leads (wires) that connect the generator to the heart. The device monitors the heart’s electrical activity and, if it detects an abnormal rhythm, it sends electrical impulses through the leads to prompt the heart to beat at a regular pace.
SEE ALSO: Where Does Blood Back Up in Left-Sided Heart Failure?
Types of Pacemakers
Single-Chamber Pacemakers: These pacemakers have one lead connected to one chamber of the heart.
Dual-Chamber Pacemakers: These have two leads, one connected to the right atrium and one to the right ventricle.
Biventricular Pacemakers (CRT-P): These are used for cardiac resynchronization therapy and have three leads, placed in the right atrium, right ventricle, and left ventricle.
Indications for Pacemaker Use
Pacemakers are commonly used to treat conditions such as:
Bradycardia: Abnormally slow heart rate.
Heart Block: A blockage in the heart’s electrical conduction system.
Atrial Fibrillation: Irregular and often rapid heart rate that can lead to poor blood flow.
Heart Failure: In cases where the heart’s electrical system is disrupted, leading to ineffective pumping of blood.
Causes of Pacemaker Failure
There are several reasons why a pacemaker might stop working, including:
Battery Depletion: Pacemaker batteries typically last 5-15 years, depending on the type and usage. When the battery depletes, the pacemaker will stop functioning.
Lead Fracture or Displacement: The leads can fracture or become dislodged, disrupting the electrical connection between the pacemaker and the heart.
Device Malfunction: This can occur due to manufacturing defects, damage during implantation, or external electromagnetic interference.
Infection: Infections around the pacemaker site can damage the device or its connections.
Electromagnetic Interference (EMI): External electromagnetic fields from certain electronic devices or medical procedures can interfere with pacemaker function.
Immediate Effects of Pacemaker Failure
If a pacemaker stops working, the immediate effects depend on the underlying heart condition for which the device was implanted. For many individuals, a pacemaker is crucial to maintain an adequate heart rate and rhythm. Therefore, failure of the device can lead to significant and potentially life-threatening consequences.
Symptoms of Pacemaker Failure
Bradycardia: If the pacemaker was implanted to treat slow heart rates, its failure can result in a return of bradycardia.
Symptoms include dizziness, fatigue, shortness of breath, fainting, and in severe cases, cardiac arrest.
Arrhythmias: The heart may revert to its abnormal rhythm, causing palpitations, chest pain, and other symptoms associated with arrhythmias.
Heart Failure Symptoms: For those with heart failure, pacemaker failure can exacerbate symptoms such as fluid retention, swelling, shortness of breath, and fatigue.
What Happens If Your Pacemaker Stops
If a pacemaker stops, it’s crucial to seek immediate medical attention.
Symptoms such as dizziness, chest pain, shortness of breath, or fainting warrant calling emergency services. In a medical setting, healthcare providers can use external pacing or medications to stabilize the heart rate and rhythm until the pacemaker can be repaired or replaced.
Long-Term Consequences
The long-term consequences of pacemaker failure depend on the duration of the failure, the speed of intervention, and the underlying heart condition. Delayed treatment can result in severe complications, including permanent damage to the heart or other organs due to inadequate blood flow.
Impact on Heart Function
Prolonged periods without adequate pacing can lead to:
Worsening Heart Failure: Inefficient heart pumping can lead to a buildup of fluids in the lungs, liver, and other organs.
Cognitive Impairment: Chronic low cardiac output can affect brain function, leading to confusion, memory issues, and other cognitive problems.
Organ Damage: Reduced blood flow to organs can cause ischemia, leading to damage and dysfunction in organs such as the kidneys and liver.
Diagnosis And Management of Pacemaker Failure
Diagnostic Steps
Interrogation of the Pacemaker: This involves using a specialized device to communicate with the pacemaker and retrieve dits function.
Electrocardiogram (ECG): An ECG can help determine the heart’s electrical activity and identify abnormalities in rhythm.
Imaging Studies: Chest X-rays or other imaging modalities can assess the position of the leads and the integrity of the device.
Management Options
Battery Replacement: If the battery is depleted, a surgical procedure is performed to replace the pulse generator.
Lead Revision: If a lead is fractured or displaced, it may be repositioned or replaced.
Device Replacement: In cases of device malfunction, the pacemaker may need to be entirely replaced.
Preventive Measures
Regular Follow-ups: Routine check-ups with a cardiologist to monitor pacemaker function and battery life.
Avoiding EMI: Patients should be educated on avoiding sources of electromagnetic interference, such as certain electronic devices and medical procedures.
Infection Prevention: Maintaining good hygiene and monitoring for signs of infection around the pacemaker site.
Living with A Pacemaker
Living with a pacemaker requires some adjustments and precautions, but many individuals can lead normal, active lives.
Here are some tips for managing life with a pacemaker:
Activity and Exercise: Most patients can engage in regular physical activity, but should avoid contact sports and heavy lifting that could dislodge the pacemaker leads.
Travel Considerations: Pacemaker patients can travel, but should carry a pacemaker ID card and be aware of airport security procedures that may involve metal detectors or body scanners.
Medical Procedures: Always inform healthcare providers about the pacemaker before undergoing any medical procedure, as certain treatments, like MRI scans, may require special precautions or alternative imaging methods.
Emotional And Psychological Impact
The knowledge that a pacemaker is life-sustaining can be a source of anxiety for some patients. Support from healthcare providers, counseling, and support groups can be beneficial in managing these feelings and maintaining a positive outlook.
Conclusion
A pacemaker is a critical device for many individuals with heart rhythm disorders, and its failure can have significant, immediate, and long-term consequences. Understanding the potential causes of pacemaker failure, recognizing the symptoms, and knowing the appropriate actions to take are vital for patients and their caregivers.