Left-sided heart failure, also known as left ventricular failure, is a condition where the left ventricle of the heart is unable to pump blood effectively throughout the body. This leads to a cascade of physiological effects, including significant impacts on kidney function and filtration. Understanding these interactions is crucial for healthcare providers and patients alike to manage and treat this complex condition effectively.
The Heart-Kidney Connection
The heart and kidneys are intricately connected through their roles in maintaining homeostasis. The heart pumps oxygenated blood to the kidneys, where filtration processes remove waste products and excess fluids, maintaining electrolyte balance and blood pressure. When the heart’s pumping ability is compromised, as in left-sided heart failure, this delicate balance is disrupted.
Pathophysiology of Left-Sided Heart Failure
Left-sided heart failure typically arises from conditions that damage or overburden the left ventricle, such as coronary artery disease, hypertension, or myocardial infarction. When the left ventricle fails to pump efficiently, blood backs up into the pulmonary circulation, leading to pulmonary congestion and edema. This backlog of blood increases the pressure within the pulmonary veins, subsequently affecting the pressure and volume dynamics in the right side of the heart and the systemic circulation.
SEE ALSO: What Happens If The Right Ventricle Fails
How Does Left Sided Heart Failure Affect Kidney Filtration?
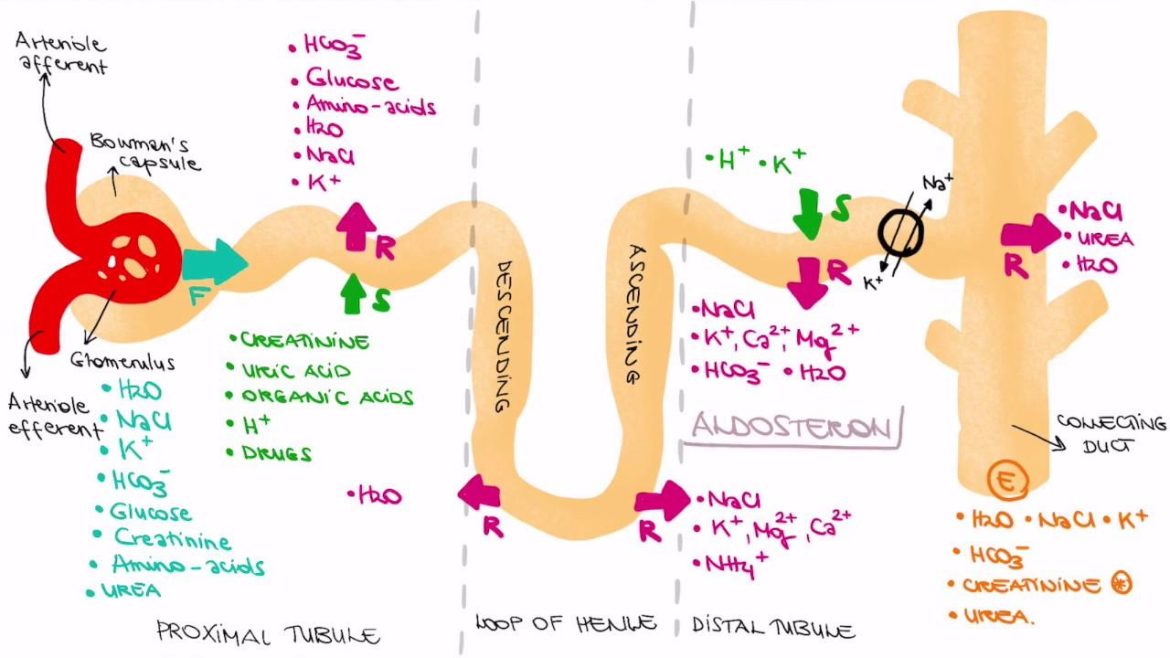
The kidneys rely on a constant supply of oxygenated blood to perform their filtration functions. In left-sided heart failure, reduced cardiac output results in diminished renal perfusion. This decrease in blood flow to the kidneys triggers several compensatory mechanisms:
Activation of the Renin-Angiotensin-Aldosterone System (RAAS): Reduced renal blood flow stimulates the release of renin from the juxtaglomerular cells in the kidneys. Renin converts angiotensinogen to angiotensin I, which is subsequently converted to angiotensin II. Angiotensin II is a potent vasoconstrictor and stimulates the release of aldosterone from the adrenal glands. Aldosterone promotes sodium and water retention to increase blood volume and pressure.
Sympathetic Nervous System Activation: Decreased cardiac output also activates the sympathetic nervous system, increasing heart rate and vasoconstriction to maintain blood pressure and perfusion to vital organs, including the kidneys.
Antidiuretic Hormone (ADH) Release: The reduced perfusion pressures and increased osmolarity sensed by the hypothalamus stimulate the release of ADH, which increases water reabsorption in the kidneys, further contributing to fluid retention.
Consequences of Compensatory Mechanisms
While these compensatory mechanisms aim to preserve kidney function and maintain blood pressure, they also have detrimental effects, particularly in the context of chronic heart failure:
Fluid Retention and Congestion: The RAAS and ADH-driven fluid retention leads to increased blood volume and venous pressures, exacerbating pulmonary and systemic congestion. This further impairs cardiac function and renal perfusion, creating a vicious cycle.
Glomerular Filtration Rate (GFR) Reduction: The increased systemic vascular resistance and reduced renal perfusion pressure decrease the glomerular filtration rate (GFR). Lower GFR means less blood is filtered through the kidneys, reducing their ability to eliminate waste products and excess fluid.
Worsening Renal Function: Prolonged reduced perfusion and increased pressures can lead to renal hypoxia, ischemia, and ultimately chronic kidney disease (CKD). The interplay between heart failure and kidney dysfunction is often referred to as the cardiorenal syndrome, highlighting their bidirectional relationship.
Clinical Manifestations
Patients with left-sided heart failure often present with symptoms related to both cardiac and renal dysfunction:
Edema: Peripheral and pulmonary edema are common due to fluid retention. This can manifest as swelling in the legs, ankles, and abdomen, as well as difficulty breathing, especially when lying down (orthopnea) or during exertion.
Reduced Urine Output: Decreased renal perfusion and activation of fluid-retaining mechanisms often lead to oliguria (reduced urine output).
Elevated Blood Pressure: Compensatory mechanisms to maintain perfusion pressure can lead to hypertension, further burdening the heart and kidneys.
Fatigue and Weakness: Reduced cardiac output and the buildup of metabolic waste products contribute to general feelings of fatigue and weakness.
Diagnostic Considerations
Diagnosing the impact of left-sided heart failure on kidney filtration involves a combination of clinical assessment, laboratory tests, and imaging studies:
Blood Tests: Elevated levels of blood urea nitrogen (BUN) and creatinine indicate impaired kidney function. Electrolyte imbalances, such as hyperkalemia, may also be present.
Urinalysis: Proteinuria (presence of protein in the urine) and changes in urine concentration can provide clues about renal dysfunction.
Imaging: Echocardiography assesses cardiac function and structure, while renal ultrasound can evaluate kidney size, structure, and blood flow.
Biomarkers: N-terminal pro-brain natriuretic peptide (NT-proBNP) or B-type natriuretic peptide (BNP) levels are often elevated in heart failure and correlate with the severity of the condition.
Management Strategies
Managing the interplay between left-sided heart failure and kidney filtration requires a multifaceted approach:
Optimizing Heart Function: Treatments to improve cardiac output and reduce congestion include angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and diuretics. These medications help reduce the workload on the heart and alleviate fluid retention.
Monitoring Fluid Balance: Careful monitoring of fluid intake and output, along with daily weight measurements, helps manage fluid retention and prevent exacerbations of heart failure.
Addressing Renal Function: Adjusting medication dosages based on renal function, avoiding nephrotoxic drugs, and managing electrolyte imbalances are crucial. In severe cases, renal replacement therapy (dialysis) may be necessary.
Lifestyle Modifications: Dietary changes, such as reducing sodium and fluid intake, can help manage symptoms. Regular physical activity, tailored to the patient’s abilities, can improve overall cardiovascular health.
Treating Underlying Conditions: Managing comorbid conditions like hypertension, diabetes, and coronary artery disease is essential to prevent further deterioration of heart and kidney function.
Conclusion
Left-sided heart failure significantly impacts kidney filtration through complex hemodynamic and neurohormonal interactions. The reduced cardiac output and compensatory mechanisms aimed at preserving renal perfusion can ultimately lead to worsening renal function and the development of cardiorenal syndrome. A comprehensive, multidisciplinary approach to managing both heart failure and kidney dysfunction is crucial for optimizing patient outcomes and improving quality of life. Understanding the intricate relationship between the heart and kidneys allows healthcare providers to tailor treatments and interventions effectively, addressing both conditions simultaneously.