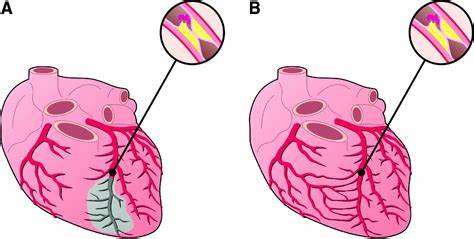
Coronary artery occlusion, also known as coronary artery disease (CAD), is a serious condition that occurs when the blood vessels supplying the heart muscle become narrowed or blocked. This blockage restricts blood flow, reducing the oxygen supply to the heart muscle, which can lead to chest pain (angina), heart attacks, and other cardiovascular complications.
Early detection and management of coronary artery occlusion are crucial for preventing severe outcomes. Here are six signs that may indicate coronary artery occlusion.
6 Signs of Coronary Artery Occlusion
1. Chest Pain (Angina)
Chest pain, also known as angina, is the most common and recognizable symptom of coronary artery occlusion. Angina typically manifests as a feeling of pressure, tightness, or squeezing in the chest. It can also present as a burning sensation or discomfort in the chest. This pain often radiates to the shoulders, arms, neck, jaw, or back. There are two primary types of angina:
Stable Angina: This type of chest pain occurs predictably with physical exertion or emotional stress and typically subsides with rest or medication. Stable angina indicates that the coronary arteries are narrowed but not completely blocked.
Unstable Angina: This is a more severe form of angina that occurs unpredictably, even at rest. Unstable angina is a medical emergency and may indicate that a coronary artery is on the verge of complete blockage or has already become blocked.
see also: 6 Typical Symptoms of Coronary Heart Disease in Women
2. Shortness of Breath
Shortness of breath, or dyspnea, is another common symptom of coronary artery occlusion. This symptom occurs because the heart is not receiving enough oxygen-rich blood to meet its needs, leading to a build-up of pressure in the heart and lungs.
As a result, fluid may accumulate in the lungs (pulmonary congestion), making it difficult to breathe. Shortness of breath may occur during physical activity, at rest, or even while lying down. In some cases, it may be accompanied by wheezing or a persistent cough.
3. Fatigue
Unexplained fatigue is a less specific but significant symptom of coronary artery occlusion. When the heart is unable to pump blood efficiently due to blocked arteries, the body’s tissues and organs receive less oxygen and nutrients. This can lead to a general feeling of tiredness and lack of energy.
Fatigue associated with coronary artery occlusion may be particularly noticeable during physical activities that were previously manageable without difficulty. In some cases, fatigue may be the only symptom, especially in women and older adults.
4. Nausea and Sweating
Nausea and sweating are often overlooked but important signs of coronary artery occlusion. These symptoms can occur due to the body’s response to the stress of inadequate blood flow to the heart.
Nausea may be accompanied by vomiting, and sweating may be profuse and unexplained, often described as a cold sweat.
These symptoms are more common during a heart attack but can also occur with angina. It’s important to note that these symptoms can be mistaken for gastrointestinal issues, so it’s crucial to consider them in the context of other signs of coronary artery occlusion.
5. Palpitations
Palpitations, or the sensation of an irregular or rapid heartbeat, can be a sign of coronary artery occlusion. When the heart muscle is deprived of oxygen, it can lead to abnormal electrical activity and arrhythmias (irregular heart rhythms).
Palpitations may feel like a fluttering, pounding, or racing sensation in the chest. While palpitations can be caused by various factors, such as stress or caffeine consumption, they should not be ignored, especially if they occur in conjunction with other symptoms of coronary artery occlusion.
6. Dizziness or Lightheadedness
Dizziness or lightheadedness can occur when the heart’s ability to pump blood effectively is compromised due to blocked coronary arteries. This can lead to a decrease in blood flow to the brain, resulting in feelings of dizziness or faintness. In severe cases, it may cause a person to lose consciousness (syncope). These symptoms can be particularly alarming and may indicate a serious reduction in cardiac output. If dizziness or lightheadedness is experienced along with chest pain or other signs of coronary artery occlusion, immediate medical attention is necessary.
Understanding The Risk Factors
Recognizing the signs of coronary artery occlusion is essential, but understanding the risk factors can also help in early detection and prevention. Common risk factors for coronary artery occlusion include:
Age: The risk increases with age, particularly for men over 45 and women over 55.
Family History: A family history of heart disease can increase the risk.
High Blood Pressure: Hypertension can damage the arteries, making them more susceptible to blockage.
High Cholesterol: Elevated levels of cholesterol can lead to plaque build-up in the arteries.
Smoking: Smoking damages the blood vessels and increases the risk of coronary artery occlusion.
Diabetes: Diabetes increases the risk of cardiovascular disease.
Obesity: Excess weight can contribute to other risk factors, such as high blood pressure, diabetes, and high cholesterol.
Physical Inactivity: A sedentary lifestyle is a significant risk factor for heart disease.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, and sodium can contribute to coronary artery occlusion.
Stress: Chronic stress may damage the arteries and increase the risk of heart disease.
Diagnosis And Treatment
If you experience any of the signs of coronary artery occlusion, it is crucial to seek medical attention promptly. Early diagnosis and treatment can significantly improve outcomes. Common diagnostic tests for coronary artery occlusion include:
Electrocardiogram (ECG): This test records the electrical activity of the heart and can detect abnormal rhythms and areas of reduced blood flow.
Stress Testing: This involves exercising or taking medication to make the heart work harder while monitoring its activity.
Echocardiogram: An ultrasound of the heart that can show how well the heart is pumping and identify areas with poor blood flow.
Coronary Angiography: A dye is injected into the coronay arteries, and X-ray images are taken to visualize blockages.
Blood Tests: These can detect markers of heart damage, such as troponin.
Treatment options for coronary artery occlusion depend on the severity of the condition and may include:
Lifestyle Changes: Improving diet, increasing physical activity, quitting smoking, and managing stress can help reduce the risk.
Medications: These may include antiplatelet drugs (such as aspirin), cholesterol-lowering medications (statins), beta-blockers, and nitroglycerin.
Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inflating a small balloon inside the artery to widen it and placing a stent to keep it open.
Coronary Artery Bypass Grafting (CABG): In this surgical procedure, a blood vessel from another part of the body is used to create a bypass around the blocked artery.
Conclusion
Coronary artery occlusion is a serious condition that requires prompt recognition and management. The six signs of coronary artery occlusion—chest pain, shortness of breath, fatigue, nausea and sweating, palpitations, and dizziness or lightheadedness—are critical indicators that should not be ignored. Understanding these signs, along with the risk factors, can help in early detection and treatment, ultimately improving the quality of life and outcomes for those affected by this condition.