Myocarditis, an inflammation of the heart muscle (myocardium), can vary widely in its severity and outcomes. This condition can be triggered by a variety of factors, including viral infections, autoimmune diseases, and exposure to certain toxins. Understanding the fatality rate of myocarditis is crucial for both medical professionals and patients, as it underscores the importance of early diagnosis and appropriate treatment. This article delves into the fatality rates associated with myocarditis, exploring the factors that influence these outcomes and highlighting the importance of timely medical intervention.
Understanding Myocarditis
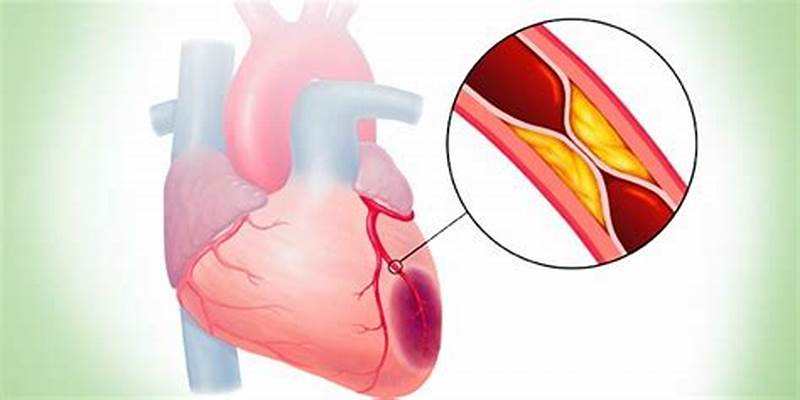
Myocarditis is an inflammatory condition of the myocardium, the muscular tissue of the heart. This inflammation can disrupt the heart’s ability to pump blood effectively, potentially leading to severe complications such as heart failure, arrhythmias, and sudden cardiac death. The causes of myocarditis are diverse and can include:
Viral infections: The most common cause, with viruses such as Coxsackievirus, Adenovirus, and more recently, SARS-CoV-2 (the virus responsible for COVID-19).
Bacterial infections: Less common but can include bacteria like Staphylococcus and Streptococcus.
Autoimmune diseases: Conditions such as lupus and giant cell arteritis can cause the immune system to attack the heart muscle.
Toxins and drugs: Certain medications, illegal drugs, and environmental toxins can also lead to myocarditis.
SEE ALSO: How Long After COVID-19 Does Myocarditis Occur?
Symptoms And Diagnosis
Symptoms of myocarditis can range from mild to severe and may include chest pain, fatigue, shortness of breath, and palpitations. In severe cases, symptoms may escalate to heart failure or sudden cardiac arrest. Diagnosis typically involves a combination of medical history, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG): To detect abnormal heart rhythms.
Echocardiogram: To assess the heart’s structure and function.
Cardiac MRI: To provide detailed images of the heart muscle and identify inflammation.
Blood tests: To check for markers of inflammation and infection.
Endomyocardial biopsy: In rare cases, a small sample of heart tissue may be taken for analysis.
Fatality Rate of Myocarditis
The fatality rate of myocarditis can be influenced by several factors, including the underlying cause, the severity of the inflammation, and the promptness of treatment. Studies have shown that the mortality rate for myocarditis varies widely:
Acute Myocarditis
Acute myocarditis, which presents suddenly and can be severe, has a variable prognosis. Studies suggest that the mortality rate for acute myocarditis ranges from 10% to 30%. The wide range is due to differences in the study populations, diagnostic criteria, and healthcare systems. In some cases, acute myocarditis can lead to fulminant myocarditis, a severe form that progresses rapidly and can be fatal without aggressive treatment.
Chronic Myocarditis
Chronic myocarditis, characterized by persistent inflammation, has a lower immediate mortality rate compared to acute myocarditis. However, it can lead to long-term complications such as dilated cardiomyopathy, which can increase the risk of heart failure and sudden cardiac death. The long-term mortality rate for chronic myocarditis is estimated to be around 10% to 20%, depending on the severity and progression of the disease.
Fulminant Myocarditis
Fulminant myocarditis is a rare but severe form of the disease that presents with rapid onset of heart failure and shock.
Despite its severity, some studies suggest that with prompt and aggressive treatment, the survival rate can be quite high, with long-term survival rates approaching 90%. However, without timely intervention, the fatality rate can be as high as 50% to 70%.
Myocarditis in COVID-19
The COVID-19 pandemic has brought attention to myocarditis as a potential complication of SARS-CoV-2 infection. While the incidence of myocarditis in COVID-19 patients is relatively low, the fatality rate can be significant, particularly in severe cases. Early studies indicated a mortality rate of around 5% to 10% in hospitalized COVID-19 patients with myocarditis, although these figures may vary as more data becomes available.
Factors Influencing Fatality Rates
Several factors can influence the fatality rate of myocarditis:
Age and Health Status
Younger individuals and those with no underlying health conditions tend to have better outcomes compared to older adults or those with pre-existing conditions such as diabetes, hypertension, or chronic kidney disease. Children and adolescents, although less frequently affected, can also experience severe myocarditis, particularly in the context of viral infections.
Cause of Myocarditis
The underlying cause of myocarditis plays a significant role in determining the outcome. Viral myocarditis, particularly when caused by common viruses like Coxsackievirus, generally has a better prognosis compared to myocarditis caused by autoimmune diseases or exposure to toxins.
Promptness of Diagnosis and Treatment
Early diagnosis and timely treatment are crucial in reducing the fatality rate of myocarditis. Delays in seeking medical care or misdiagnosis can lead to worse outcomes. Treatment options may include medications to reduce inflammation, manage heart failure symptoms, and control arrhythmias, as well as advanced therapies such as mechanical circulatory support or heart transplantation in severe cases.
Severity of Inflammation
The degree of inflammation and the extent of damage to the heart muscle can also impact the prognosis. Mild cases of myocarditis may resolve with minimal treatment, while severe inflammation can lead to significant cardiac dysfunction and an increased risk of fatal outcomes.
Treatment And Management
The treatment of myocarditis aims to address the underlying cause, reduce inflammation, and manage symptoms.
Treatment strategies can vary depending on the severity of the disease and may include:
Medications
Anti-inflammatory drugs: Such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to reduce inflammation.
Antiviral or antibiotic therapy: If a specific infectious agent is identified.
Heart failure medications: Including ACE inhibitors, beta-blockers, and diuretics to manage heart failure symptoms.
Immunosuppressive therapy: For autoimmune causes of myocarditis.
Lifestyle Modifications
Patients with myocarditis are often advised to limit physical activity to reduce the strain on the heart. A low-sodium diet may be recommended to help manage heart failure symptoms.
Advanced Therapies
In severe cases, more aggressive treatments may be necessary, including:
Mechanical circulatory support: Such as ventricular assist devices (VADs) or extracorporeal membrane oxygenation (ECMO) for patients with severe heart failure.
Heart transplantation: In cases of refractory heart failure where other treatments have failed.
Conclusion
Myocarditis is a complex and potentially life-threatening condition with a variable prognosis. The fatality rate of myocarditis can range from as low as 5% in mild cases to as high as 70% in severe, fulminant cases without treatment.
Factors such as age, overall health, underlying cause, and promptness of treatment play crucial roles in determining the outcome. Early diagnosis and appropriate management are key to improving survival rates and reducing the long-term impact of this condition. As research continues, our understanding of myocarditis and its treatment will evolve, hopefully leading to better outcomes for patients affected by this challenging disease.