Pulseless ventricular fibrillation (VF) is a critical cardiac emergency characterized by erratic, disorganized electrical activity in the ventricles of the heart, leading to an ineffective quivering of the heart muscle rather than coordinated contractions.
This condition results in the cessation of effective blood circulation, rendering the heart unable to pump blood to vital organs, including the brain and lungs. Understanding the pathophysiology, causes, diagnosis, and treatment of pulseless ventricular fibrillation is crucial for medical professionals and anyone interested in cardiovascular health.
Pathophysiology of Pulseless Ventricular Fibrillation
Pulseless ventricular fibrillation occurs when the electrical signals that regulate the heart’s rhythm become chaotic. The heart’s normal rhythm is controlled by a sequence of electrical impulses that originate in the sinoatrial (SA) node, spread through the atria, pass through the atrioventricular (AV) node, and travel through the His-Purkinje system to stimulate the ventricles. In VF, this orderly conduction pathway is disrupted, leading to rapid, irregular electrical impulses that cause the ventricles to quiver instead of contract.
SEE ALSO: 5 Ways to Treat Spinal Hypotension
Electrical Conduction and Its Disruption
Normal Conduction Pathway:
The SA node generates an impulse.
The impulse travels through the atria, causing them to contract.
The impulse reaches the AV node, which delays the signal slightly.
The impulse travels through the His bundle, bundle branches, and Purkinje fibers, leading to coordinated ventricular contraction.
Disruption in VF:
Multiple reentrant circuits form within the ventricles.
Rapid, unsynchronized electrical impulses cause the heart muscle to quiver.
The lack of coordinated contraction leads to ineffective blood pumping.
Consequences of Ventricular Fibrillation
Without effective ventricular contraction, the heart cannot pump blood, leading to:
Systemic Hypoperfusion: Insufficient blood flow to organs and tissues.
Hypoxia: Lack of oxygen delivery to vital organs, including the brain.
Acidosis: Accumulation of acid in the blood due to inadequate removal of carbon dioxide.
Cellular Death: Irreversible damage to cells, particularly in the brain and heart.
Causes And Risk Factors
Pulseless ventricular fibrillation can arise from various underlying conditions and triggers, often related to structural heart disease, ischemic events, or electrolyte imbalances.
Common Causes
Coronary Artery Disease (CAD):
Myocardial infarction (heart attack) is a leading cause.
Ischemia-induced electrical instability can precipitate VF.
Cardiomyopathies:
Hypertrophic cardiomyopathy (HCM) and dilated cardiomyopathy (DCM) can predispose individuals to VF.
Congenital Heart Disorders:
Genetic conditions like Long QT Syndrome (LQTS) and Brugada Syndrome increase VF risk.
Electrolyte Imbalances:
Hypokalemia (low potassium) and hyperkalemia (high potassium) can disrupt cardiac conduction.
Hypomagnesemia (low magnesium) and hypercalcemia (high calcium) also contribute.
Medications and Toxins:
Antiarrhythmic drugs, especially those prolonging the QT interval.
Recreational drugs like cocaine and methamphetamine.
Risk Factors
Previous Cardiac Events:
History of myocardial infarction or previous episodes of VF.
Family History:
Genetic predisposition to arrhythmias.
Lifestyle Factors:
Smoking, excessive alcohol consumption, and drug abuse.
Chronic Conditions:
Diabetes, hypertension, and obesity.
Clinical Presentation And Diagnosis
Pulseless ventricular fibrillation is typically identified in emergency settings due to its sudden onset and life-threatening nature.
Clinical Presentation
Sudden Collapse:
The patient often experiences a sudden loss of consciousness and collapse.
Absence of Pulse:
No palpable pulse due to ineffective cardiac output.
Unresponsiveness:
The patient is unresponsive and may exhibit agonal gasping or apnea.
No Effective Heart Sounds:
Auscultation reveals the absence of heart sounds.
Diagnostic Tools
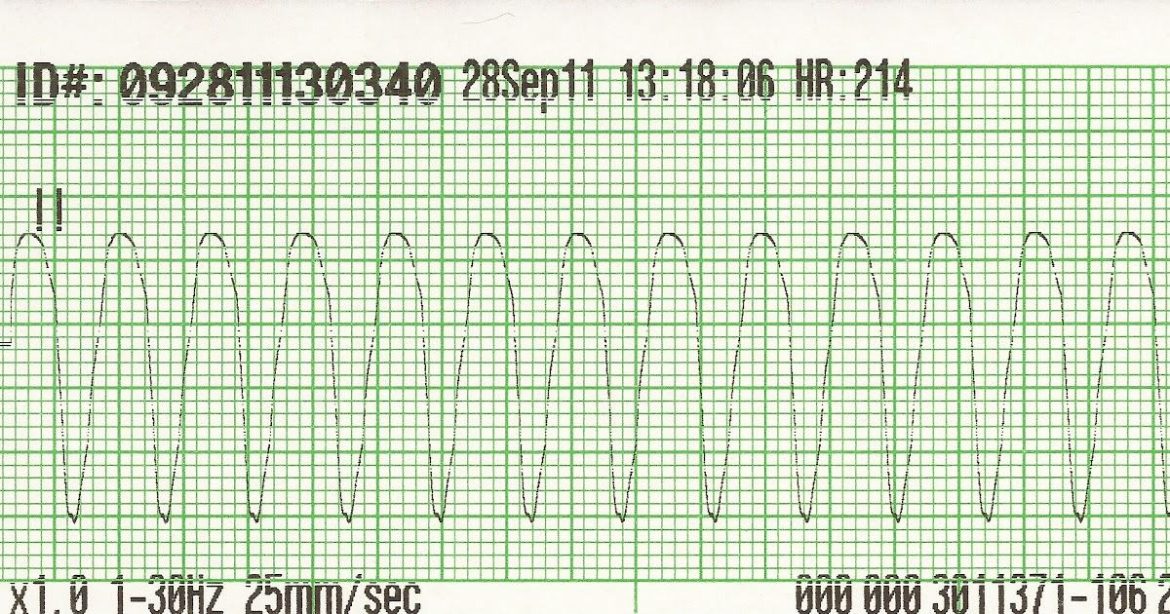
Electrocardiogram (ECG):
The primary tool for diagnosing VF.
Characteristic findings include rapid, irregular, and chaotic electrical activity without discernible QRS complexes.
Defibrillator Monitors:
Used in emergency settings to confirm VF.
Provide real-time feedback on rhythm and the effectiveness of interventions.
Cardiac Biomarkers:
Blood tests for troponin levels to assess for underlying myocardial infarction.
Imaging Studies:
Echocardiography to evaluate structural heart disease.
Coronary angiography if CAD is suspected.
Treatment And Management
Immediate intervention is critical to prevent irreversible organ damage and improve survival outcomes.
Initial Management
Basic Life Support (BLS):
Initiate cardiopulmonary resuscitation (CPR) with chest compressions and rescue breaths.
Ensure high-quality compressions at a rate of 100-120 per minute and a depth of 2-2.4 inches.
Advanced Cardiac Life Support (ACLS):
Rapid defibrillation is the definitive treatment for VF.
Administer a biphasic shock of 120-200 Joules or a monophasic shock of 360 Joules.
Continue CPR immediately after defibrillation and reassess the rhythm.
Pharmacological Interventions
Epinephrine:
Administer 1 mg intravenously every 3-5 minutes during CPR to enhance coronary and cerebral perfusion.
Antiarrhythmic Drugs:
Amiodarone: 300 mg IV bolus, followed by 150 mg if VF persists.
Lidocaine: An alternative if amiodarone is unavailable, with a dose of 1-1.5 mg/kg IV.
Conclusion
Pulseless ventricular fibrillation is a life-threatening cardiac arrhythmia requiring immediate medical intervention.
Understanding its pathophysiology, causes, and treatment options is essential for effective management and improving patient outcomes. Advances in emergency care, along with preventive strategies and long-term management, play crucial roles in reducing the incidence and mortality associated with this condition. By recognizing the signs and implementing timely interventions, healthcare providers can make a significant difference in the survival and recovery of individuals affected by pulseless ventricular fibrillation.