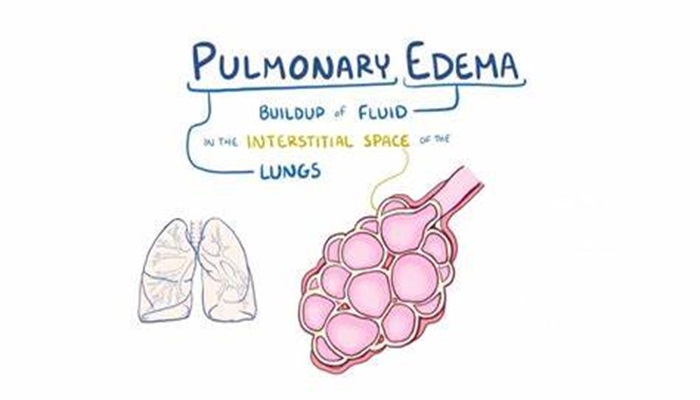
Pulmonary edema is a significant and often life-threatening condition that arises as a complication of left-sided heart failure. Understanding its causes is crucial for effective management and treatment. This article explores the six main causes of pulmonary edema in left-sided heart failure, providing a comprehensive overview of the mechanisms involved.
The Pathophysiology of Left-Sided Heart Failure
Left-sided heart failure occurs when the left ventricle cannot maintain adequate cardiac output. This failure can manifest in two forms: systolic heart failure, characterized by a reduced ejection fraction, and diastolic heart failure, where the heart’s filling is impaired despite a preserved ejection fraction. Both conditions can lead to fluid accumulation in the lungs due to increased hydrostatic pressure in the pulmonary capillaries.
see also: How Does Left Sided Heart Failure Affect Kidney Filtration?
Mechanisms Leading to Pulmonary Edema
The development of pulmonary edema in left-sided heart failure is multifactorial, primarily involving hemodynamic changes, neurohormonal activation, and increased vascular permeability. Below, we discuss the six main causes that contribute to the onset of pulmonary edema in this clinical scenario.
1. Increased Pulmonary Capillary Hydrostatic Pressure
One of the primary mechanisms behind pulmonary edema in left-sided heart failure is the increase in pulmonary capillary hydrostatic pressure. When the left ventricle fails, blood backs up into the left atrium and subsequently into the pulmonary veins. This backlog raises the pressure within the pulmonary capillaries, leading to fluid leakage into the interstitial space and ultimately into the alveoli.
Pathophysiological Implications
Increased Pressure: Elevated pressures can reach thresholds that exceed the oncotic pressure gradient, resulting in fluid transudation.
Symptomatic Presentation: Patients may present with dyspnea, orthopnea, and paroxysmal nocturnal dyspnea due to fluid accumulation.
2. Increased Vascular Permeability
In addition to increased hydrostatic pressure, increased vascular permeability plays a critical role in the development of pulmonary edema. In heart failure, various factors can lead to the alteration of the endothelial barrier, making it more permeable to fluid and proteins.
Factors Contributing to Increased Permeability
Cytokine Release: Inflammatory cytokines released during heart failure can damage the endothelial lining, increasing permeability.
Ischemia: Reduced blood flow can lead to local hypoxia and inflammation, further compromising vascular integrity.
Clinical Manifestations
The result of increased permeability is often a mixed picture of pulmonary edema characterized by both transudative and exudative fluid characteristics, complicating the clinical management.
3. Neurohormonal Activation
Left-sided heart failure triggers significant neurohormonal responses, which are essential for compensating for decreased cardiac output. However, these compensatory mechanisms can paradoxically lead to pulmonary edema.
Key Hormones Involved
Renin-Angiotensin-Aldosterone System (RAAS): Activation of this system results in increased sodium and water retention, leading to volume overload.
Sympathetic Nervous System (SNS): Increased adrenergic tone leads to vasoconstriction and elevated systemic vascular resistance, further straining the left ventricle.
Consequences
While these responses aim to stabilize hemodynamics, they can increase the workload of the heart, exacerbating pulmonary congestion and edema over time.
4. Left Ventricular Compliance
Left ventricular compliance refers to the ability of the ventricle to stretch and fill adequately during diastole. In conditions such as diastolic heart failure (heart failure with preserved ejection fraction), poor compliance can significantly contribute to pulmonary edema.
Impact of Poor Compliance
Diastolic Dysfunction: Impaired relaxation and filling of the left ventricle lead to elevated left atrial pressures, which subsequently increases pulmonary capillary pressure.
Symptoms of Pulmonary Congestion: Patients often experience similar symptoms to those with systolic dysfunction, including shortness of breath and pulmonary edema.
Management Implications
Recognizing diastolic dysfunction is vital for appropriate management strategies, which may include diuretics and afterload reduction to alleviate symptoms.
5. High Cardiac Output States
In certain conditions, even patients with left-sided heart failure may experience high cardiac output states that can lead to pulmonary edema. These situations are typically seen in cases such as severe anemia, hyperthyroidism, or arteriovenous fistulas.
Mechanisms at Play
Increased Blood Volume: A high output can lead to volume overload, causing increased pulmonary capillary pressures.
Compensatory Mechanisms: While the heart attempts to compensate for increased demands, the resultant hemodynamic changes may predispose patients to pulmonary edema.
Clinical Relevance
Recognizing high output states is essential for the holistic management of patients with left-sided heart failure to prevent complications such as pulmonary edema.
6. Non-Cardiac Causes of Pulmonary Edema
Although left-sided heart failure is a leading cause of pulmonary edema, non-cardiac factors can also contribute to the condition. These include acute respiratory distress syndrome (ARDS), pneumonia, and renal failure.
Pathophysiology
ARDS: Inflammatory processes lead to increased permeability and fluid accumulation in the alveoli.
Pneumonia: Infection can cause pulmonary inflammation and resultant edema, complicating existing heart failure.
Renal Failure: Reduced renal perfusion and the resultant fluid overload can exacerbate pulmonary congestion.
Implications for Management
Understanding these non-cardiac contributors is critical in formulating a comprehensive treatment strategy for patients with pulmonary edema due to left-sided heart failure.
Conclusion
Pulmonary edema in left-sided heart failure is a complex condition arising from a combination of hemodynamic changes, neurohormonal activation, and vascular alterations. By understanding the six main causes—increased pulmonary capillary hydrostatic pressure, increased vascular permeability, neurohormonal activation, left ventricular compliance, high cardiac output states, and non-cardiac causes—clinicians can better diagnose, treat, and manage patients with this serious condition.