Arrhythmia, a condition characterized by irregular heartbeats, can significantly impact an individual’s health and quality of life. The heart’s rhythm is controlled by a complex system of electrical signals, and when this system malfunctions, it can lead to various types of arrhythmias. Understanding the underlying causes of arrhythmia is crucial for diagnosis, treatment, and prevention. This article delves into the mechanisms, risk factors, and conditions that contribute to the development of arrhythmia.
The Electrical System of the Heart
The heart’s electrical system is responsible for maintaining a consistent and regular heartbeat. This system comprises the following key components:
Sinoatrial (SA) Node: Often referred to as the heart’s natural pacemaker, the SA node is located in the right atrium. It generates electrical impulses that initiate each heartbeat.
Atrioventricular (AV) Node: Situated between the atria and ventricles, the AV node receives impulses from the SA node and delays them slightly before passing them to the ventricles. This delay ensures that the atria contract before the ventricles.
SEE ALSO: The 5 Best Causes of Arrhythmia
How Electrical Impulses Cause Heartbeats
Under normal conditions, the electrical impulses generated by the SA node travel through the atria, causing them to contract and push blood into the ventricles. The impulses then reach the AV node, which delays them slightly before they pass through the His-Purkinje network to the ventricles, causing them to contract and pump blood to the rest of the body.
This sequence of events creates a coordinated and efficient heartbeat.
What Causes Arrhythmia?
1. Structural Heart Changes
Structural abnormalities in the heart can disrupt its electrical system, leading to arrhythmias. These changes may result from:
Congenital Heart Defects: Some individuals are born with structural abnormalities that affect the heart’s normal function.
Cardiomyopathy: This condition involves changes in the heart muscle, making it thicker, stiffer, or larger than normal, which can interfere with electrical signal transmission.
Heart Valve Disorders: Malfunctioning heart valves can alter blood flow patterns, leading to electrical disturbances.
2. Coronary Artery Disease and Heart Attacks
Coronary artery disease (CAD) and heart attacks are significant contributors to arrhythmia. CAD causes the arteries that supply blood to the heart muscle to narrow or become blocked, reducing blood flow.
A heart attack, resulting from a sudden blockage of a coronary artery, can damage the heart muscle and disrupt its electrical system, leading to arrhythmias.
3. High Blood Pressure (Hypertension)
Chronic high blood pressure forces the heart to work harder, which can lead to hypertrophy (thickening of the heart muscle). This thickening can alter the heart’s electrical pathways, increasing the risk of arrhythmias.
4. Electrolyte Imbalances
Electrolytes such as potassium, calcium, and sodium play crucial roles in conducting electrical impulses in the heart.
Imbalances in these electrolytes can disrupt normal heart rhythms. For example:
Hyperkalemia: Elevated potassium levels can slow down the heart’s electrical conduction, leading to arrhythmias.
Hypokalemia: Low potassium levels can cause the heart to become overly excitable, also leading to arrhythmias.
Hypocalcemia and Hypercalcemia: Abnormal calcium levels can interfere with the contraction of heart muscles, affecting the rhythm.
5. Drug and Substance Abuse
Certain medications, illegal drugs, and excessive alcohol consumption can affect the heart’s electrical system:
Medications: Some prescription and over-the-counter medications can have side effects that include arrhythmias.
Examples include beta-blockers, calcium channel blockers, and antiarrhythmic drugs.
Stimulants: Drugs like cocaine and amphetamines can overstimulate the heart, leading to dangerous arrhythmias.
Alcohol: Chronic heavy drinking or binge drinking can damage the heart muscle and lead to arrhythmias.
6. Lifestyle Factors
Several lifestyle factors can contribute to the development of arrhythmia:
Poor Diet: Diets high in unhealthy fats, sugar, and sodium can lead to obesity, high blood pressure, and other conditions that increase the risk of arrhythmias.
Lack of Physical Activity: Sedentary lifestyles can contribute to obesity, hypertension, and other risk factors for arrhythmias.
Stress and Anxiety: High stress levels can trigger the release of hormones like adrenaline, which can increase heart rate and lead to arrhythmias.
7. Age and Genetic Factors
Age: The risk of arrhythmia increases with age, partly due to the natural aging of the heart and its electrical system.
Genetics: A family history of arrhythmias or other heart conditions can increase an individual’s risk. Certain genetic mutations can affect the heart’s electrical pathways.
Types of Arrhythmias
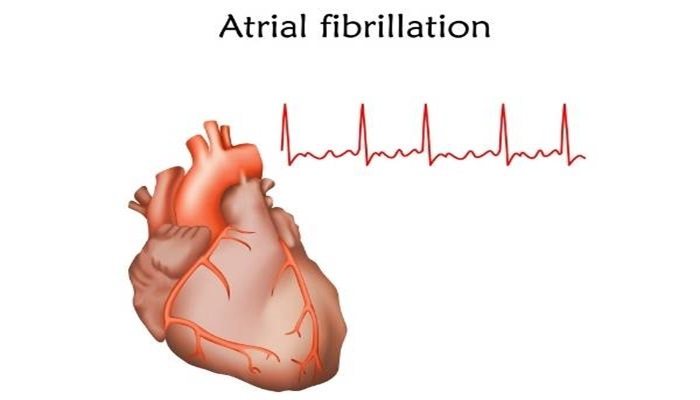
1. Atrial Fibrillation (AFib)
AFib is the most common type of arrhythmia, characterized by rapid and irregular beating of the atria. It can lead to poor blood flow, increasing the risk of stroke and heart failure. Common causes include high blood pressure, coronary artery disease, and heart valve disorders.
2. Ventricular Tachycardia (VT)
VT is a rapid heartbeat originating from the ventricles. It can be life-threatening if it prevents the heart from pumping effectively. Causes include structural heart disease, previous heart attacks, and cardiomyopathy.
3. Bradycardia
Bradycardia is a slower than normal heart rate, often caused by issues with the heart’s electrical system. It can result from aging, heart disease, or certain medications.
4. Supraventricular Tachycardia (SVT)
SVT refers to a rapid heart rate originating above the ventricles. It can be caused by abnormal electrical pathways or circuits in the heart and is often triggered by stress, caffeine, or alcohol.
5. Premature Ventricular Contractions (PVCs)
PVCs are extra heartbeats that originate in the ventricles and disrupt the regular heart rhythm. They can be caused by stress, caffeine, or electrolyte imbalances and are usually benign.
Diagnosis And Treatment
Diagnosing arrhythmias involves a combination of medical history, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart.
Holter Monitor: A portable device worn for 24-48 hours to record the heart’s electrical activity.
Event Monitor: A device worn for weeks or months to capture arrhythmias that occur infrequently.
Electrophysiological Study (EPS): Involves inserting catheters into the heart to study its electrical activity and identify abnormal areas.
Treatment options vary depending on the type and severity of the arrhythmia and may include:
Medications: Antiarrhythmic drugs, beta-blockers, calcium channel blockers, and anticoagulants.
Lifestyle Changes: Healthy diet, regular exercise, stress management, and avoiding stimulants.
Procedures: Cardioversion, catheter ablation, and implantation of devices like pacemakers and defibrillators.
Prevention And Management
Preventing and managing arrhythmias involves addressing underlying risk factors and maintaining a heart-healthy lifestyle:
Control Blood Pressure and Cholesterol: Regular monitoring and management through diet, exercise, and medications.
Healthy Diet: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats.
Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
Avoid Stimulants: Limit caffeine and avoid recreational drugs and excessive alcohol.
Manage Stress: Practice relaxation techniques such as yoga, meditation, and deep breathing.
Conclusion
Arrhythmias are caused by a variety of factors, including structural heart changes, coronary artery disease, electrolyte imbalances, lifestyle factors, and genetic predispositions. Understanding these causes is essential for effective diagnosis, treatment, and prevention. By addressing underlying risk factors and maintaining a heart-healthy lifestyle, individuals can reduce their risk of developing arrhythmias and improve their overall cardiovascular health.