Arrhythmia is a condition characterized by an irregular heartbeat, where the heart may beat too fast, too slow, or with an irregular rhythm. While many arrhythmias are harmless and can be managed with lifestyle changes or medication, others can be life-threatening and require immediate medical attention. Understanding when arrhythmia becomes dangerous is crucial for proper management and treatment. This article delves into the types of arrhythmias, their causes, symptoms, and when they pose a significant risk to health.
Understanding Arrhythmia
Arrhythmias are classified based on where they originate in the heart and their effect on heart rate. The primary types include:
Atrial Fibrillation (AFib): The most common type of arrhythmia, AFib causes the atria (upper chambers of the heart) to quiver instead of beating effectively, leading to poor blood flow.
Ventricular Tachycardia (VT): This type originates in the ventricles (lower chambers of the heart) and results in a rapid heart rate that can prevent the heart from pumping enough blood.
Ventricular Fibrillation (VFib): VFib is a chaotic heart rhythm originating in the ventricles, causing the heart to quiver ineffectively and stopping blood flow to the rest of the body.
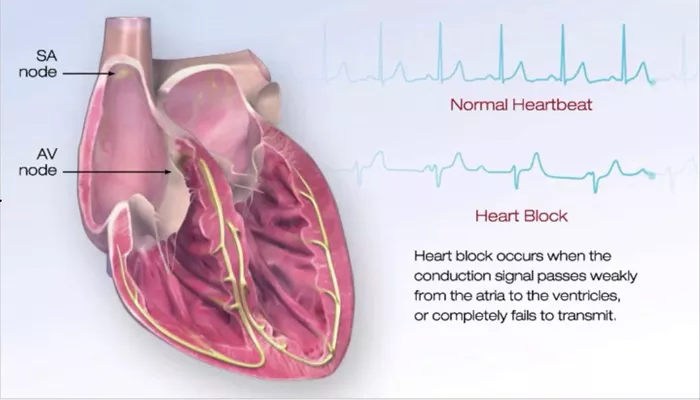
Bradyarrhythmias: These are slow heart rhythms that can result from problems with the heart’s natural pacemaker or electrical conduction system.
Causes of Arrhythmia
Arrhythmias can be caused by various factors, including:
Heart Disease: Conditions such as coronary artery disease, heart failure, and cardiomyopathy can lead to arrhythmias.
Electrolyte Imbalances: Abnormal levels of electrolytes like potassium, sodium, calcium, and magnesium can disrupt the heart’s electrical impulses.
Medications: Certain drugs, including some prescribed for heart conditions, can cause arrhythmias as a side effect.
Caffeine, Alcohol, and Nicotine: These substances can trigger arrhythmias in some individuals.
Stress and Anxiety: High stress levels and anxiety can lead to arrhythmias in susceptible people.
Genetics: Some arrhythmias are inherited and can run in families.
see also: The 6 Best Ways to Stop Heart Arrhythmias
Symptoms of Arrhythmia
The symptoms of arrhythmia can vary widely depending on the type and severity. Common symptoms include:
- Palpitations (a feeling of skipped heartbeats or fluttering)
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain or discomfort
- Fatigue
- Fainting (syncope)
When Arrhythmia Becomes Dangerous
1. Hemodynamic Instability
Arrhythmias become dangerous when they affect the heart’s ability to pump blood effectively, leading to hemodynamic instability. This can result in symptoms such as severe dizziness, fainting, low blood pressure, and shock. Hemodynamic instability is particularly concerning in arrhythmias like ventricular tachycardia and ventricular fibrillation, where the rapid heart rate prevents the heart from filling properly between beats, reducing cardiac output.
2. Risk of Stroke
Atrial fibrillation, the most common type of arrhythmia, significantly increases the risk of stroke. In AFib, the irregular and often rapid heart rate can cause blood to pool in the atria, leading to the formation of blood clots. If a clot travels to the brain, it can cause a stroke. The risk of stroke in AFib patients is influenced by factors such as age, hypertension, diabetes, and prior history of stroke.
3. Sudden Cardiac Arrest
Ventricular fibrillation is one of the most dangerous arrhythmias as it can lead to sudden cardiac arrest. In VFib, the heart’s electrical activity becomes chaotic, causing the ventricles to quiver ineffectively instead of pumping blood. This results in a sudden loss of heart function, breathing, and consciousness. Without immediate medical intervention, sudden cardiac arrest can be fatal within minutes.
4. Heart Failure
Chronic arrhythmias can contribute to the development of heart failure. Persistent arrhythmias, such as AFib, can weaken the heart muscle over time, reducing its efficiency in pumping blood. This can lead to symptoms of heart failure, including shortness of breath, fluid retention, and fatigue. Heart failure itself can also predispose individuals to developing arrhythmias, creating a vicious cycle.
5. Compromised Blood Supply to Organs
Arrhythmias can compromise the blood supply to vital organs, including the brain, kidneys, and liver. In severe cases, this can result in organ dysfunction and damage. For instance, prolonged episodes of tachycardia or bradycardia can reduce the blood flow to the brain, leading to confusion, memory problems, and even stroke.
Diagnostic Approaches
Diagnosing arrhythmias involves several approaches to determine the type, cause, and severity. These include:
Electrocardiogram (ECG): This test records the electrical activity of the heart and can identify abnormal rhythms.
Holter Monitor: A portable ECG device worn for 24-48 hours to detect intermittent arrhythmias.
Event Monitor: Similar to a Holter monitor but used for longer periods, up to 30 days, to capture sporadic arrhythmias.
Echocardiogram: An ultrasound of the heart to assess its structure and function.
Stress Test: Evaluates the heart’s response to physical exertion and can trigger arrhythmias.
Electrophysiological Study (EPS): An invasive test that maps the electrical pathways of the heart to identify the source of arrhythmias.
Treatment Options
The treatment of arrhythmias depends on the type, severity, and underlying cause. Common treatments include:
Medications: Antiarrhythmic drugs, beta-blockers, and calcium channel blockers can help control heart rate and rhythm.
Electrical Cardioversion: A procedure that uses electric shocks to restore normal heart rhythm in cases of AFib or other arrhythmias.
Catheter Ablation: A minimally invasive procedure that destroys the abnormal heart tissue causing the arrhythmia.
Pacemakers: Devices implanted to regulate slow heart rhythms (bradyarrhythmias).
Implantable Cardioverter-Defibrillators (ICDs): Devices implanted to monitor and correct life-threatening arrhythmias like VT and VFib.
Lifestyle Changes: Managing risk factors such as hypertension, diabetes, and avoiding triggers like excessive caffeine and alcohol can help control arrhythmias.
Prevention And Management
Preventing and managing arrhythmias involves addressing the underlying risk factors and maintaining a heart-healthy lifestyle. This includes:
Regular Exercise: Engaging in moderate physical activity can improve cardiovascular health and reduce the risk of arrhythmias.
Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support heart health.
Stress Management: Techniques such as mindfulness, meditation, and yoga can help reduce stress and prevent arrhythmias.
Avoiding Stimulants: Limiting the intake of caffeine, alcohol, and nicotine can reduce the likelihood of arrhythmias.
Regular Check-ups: Routine medical exams and monitoring can help detect and manage arrhythmias early.
Conclusion
Arrhythmias can range from harmless to life-threatening, and understanding when they become dangerous is essential for effective management. Hemodynamic instability, increased risk of stroke, sudden cardiac arrest, heart failure, and compromised blood supply to organs are key indicators that an arrhythmia has become dangerous. Prompt diagnosis, appropriate treatment, and preventive measures are crucial to managing arrhythmias and reducing their potential complications. By staying informed and proactive, individuals can protect their heart health and improve their overall quality of life.