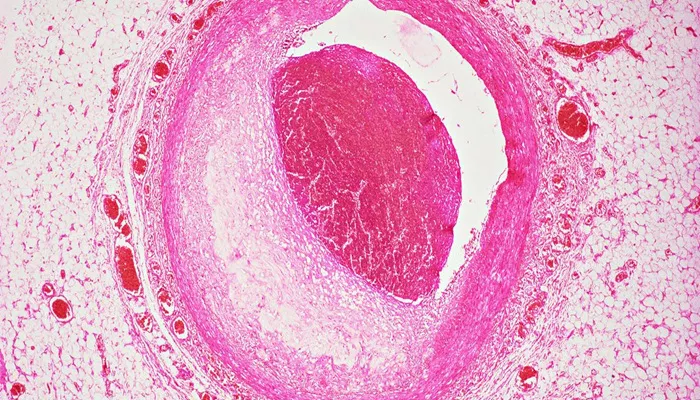
Coronary artery disease (CAD), also known as coronary heart disease (CHD), is the most common type of heart disease. It occurs when the arteries that supply blood to the heart muscle become narrowed or blocked due to the buildup of cholesterol and other materials, known as plaque. This can lead to various complications, including angina (chest pain), heart attacks, and heart failure. Understanding the different types of coronary artery disease is crucial for early diagnosis, effective treatment, and prevention. This article delves into the types of CAD, their causes, symptoms, and treatments.
What Are The Types of Coronary Artery Disease?
1. Stable Angina
Stable angina is the most common form of angina and is characterized by predictable chest pain or discomfort that typically occurs with physical exertion or stress. The pain usually lasts for a few minutes and goes away with rest or medication such as nitroglycerin. Stable angina is a sign that the heart muscle is not getting enough oxygen-rich blood during periods of increased demand.
Causes
Stable angina is usually caused by atherosclerosis, where plaque builds up on the walls of the coronary arteries, narrowing them and reducing blood flow to the heart muscle. This condition develops over time and can be exacerbated by risk factors such as high cholesterol, high blood pressure, smoking, diabetes, and a sedentary lifestyle.
Symptoms
Chest pain or discomfort, often described as pressure, squeezing, or a burning sensation.
Pain may radiate to the arms, neck, jaw, shoulder, or back.
Shortness of breath.
Fatigue, especially during physical activity.
SEE ALSO: 7 Best Treatments for Left Main Coronary Artery Occlusion
Treatment
Lifestyle changes: Adopting a heart-healthy diet, engaging in regular exercise, quitting smoking, and managing stress.
Medications: Nitroglycerin, beta-blockers, calcium channel blockers, and statins to manage symptoms and risk factors.
Medical procedures: Angioplasty with stent placement or coronary artery bypass grafting (CABG) in severe cases.
2. Unstable Angina
Unstable angina is a more serious condition than stable angina and is considered a medical emergency. It occurs when chest pain happens suddenly and unpredictably, often at rest or with minimal exertion. The pain may last longer and be more severe than that of stable angina.
Causes
Unstable angina is often caused by the rupture of an atherosclerotic plaque with subsequent formation of a blood clot that partially or completely blocks a coronary artery. This can significantly reduce or stop blood flow to the heart muscle.
Symptoms
Sudden, intense chest pain or discomfort that may not be relieved by rest or medication.
Pain that radiates to the arms, neck, jaw, shoulder, or back.
Shortness of breath.
Nausea, sweating, and lightheadedness.
Treatment
Immediate medical attention: Hospitalization is required to stabilize the condition and prevent a heart attack.
Medications: Antiplatelet agents (e.g., aspirin, clopidogrel), anticoagulants, beta-blockers, nitrates, and statins.
Medical procedures: Angioplasty with stent placement or coronary artery bypass grafting (CABG) if necessary.
3. Variant Angina (Prinzmetal’s Angina)
Variant angina, also known as Prinzmetal’s angina, is a rare form of angina that typically occurs at rest, often during the night or early morning hours. It is caused by a spasm in a coronary artery, which temporarily reduces blood flow to the heart muscle.
Causes
The exact cause of the coronary artery spasm in variant angina is not well understood, but it may be related to abnormalities in the endothelial function of the artery, increased activity of the sympathetic nervous system, or imbalance in the control of vascular tone.
Symptoms
Severe chest pain or discomfort, usually occurring at rest.
Pain that may radiate to the arms, neck, jaw, shoulder, or back.
Shortness of breath.
Palpitations or irregular heartbeats.
Treatment
Medications: Calcium channel blockers and nitrates are the primary treatments to prevent and relieve coronary artery spasms.
Lifestyle changes: Avoiding smoking, managing stress, and maintaining a heart-healthy lifestyle.
4. Microvascular Angina
Microvascular angina, also known as cardiac syndrome X or non-obstructive coronary artery disease, is a type of angina that occurs when the small blood vessels (microvasculature) in the heart do not function properly. This can cause chest pain without significant blocovascular function.
Lifestyle changes: Adopting a heart-healthy diet, regular exercise, smoking cessation, and stress management.
Monitoring and managing underlying conditions such as hypertension and diabetes.
5. Silent Ischemia
Silent ischemia refers to episodes of reduced blood flow to the heart muscle that occur without noticeable symptoms. This condition can be particularly dangerous because it may go undetected until it leads to more severe complications such as a heart attack.
Causes
Silent ischemia is often caused by the same factors that lead to other types of coronary artery disease, including atherosclerosis and coronary artery spasms. Risk factors include high cholesterol, high blood pressure, smoking, diabetes, and a family history of heart disease.
Symptoms
No noticeable symptoms during episodes of reduced blood flow.
Detection is usually through diagnostic tests such as electrocardiograms (ECGs), stress tests, or continuous ambulatory monitoring.
Treatment
Lifestyle changes: Heart-healthy diet, regular physical activity, smoking cessation, and stress management.
Medications: Beta-blockers, calcium channel blockers, nitrates, and statins to manage risk factors and prevent ischemic episodes.
Regular monitoring: Frequent check-ups and diagnostic tests to detect and manage silent ischemia.
6. Nonobstructive Coronary Artery Disease
Nonobstructive coronary artery disease is characterized by coronary arteries that appear normal or only mildly narrowed on angiograms but still cause symptoms of angina or other cardiovascular problems. This condition is more common in women and can be challenging to diagnose.
Causes
Nonobstructive CAD may be caused by endothelial dysfunction, microvascular disease, or abnormalities in coronary blood flow regulation. It can be associated with risk factors such as high cholesterol, high blood pressure, smoking, diabetes, and inflammatory conditions.
Symptoms
Chest pain or discomfort, often during physical activity or at rest.
Shortness of breath.
Fatigue.
Palpitations or irregular heartbeats.
Treatment
Lifestyle changes: Adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, and managing stress.
Medications: Beta-blockers, calcium channel blockers, nitrates, and statins to manage symptoms and risk factors.
Management of underlying conditions: Controlling hypertension, diabetes, and inflammatory conditions.
Conclusion
Coronary artery disease is a complex and multifaceted condition with various types, each with its own causes, symptoms, and treatments. Understanding these different types is essential for effective diagnosis, management, and prevention. By adopting a heart-healthy lifestyle, managing risk factors, and seeking timely medical attention, individuals can significantly reduce their risk of developing CAD and improve their overall cardiovascular health. Regular check-ups and monitoring are crucial, especially for those with a family history of heart disease or other risk factors.