Hypertension, commonly known as high blood pressure, is a prevalent health condition that affects millions worldwide. It’s a complex disorder with multiple contributing factors, including genetics, lifestyle, and underlying medical conditions. One of the less commonly discussed causes of hypertension is low renin levels. Renin is an enzyme secreted by the kidneys that plays a critical role in the body’s blood pressure regulation system. Understanding how low renin can lead to hypertension is crucial for identifying and managing this specific subtype of the condition.
Renin And Its Role in Blood Pressure Regulation
Renin is a key component of the renin-angiotensin-aldosterone system (RAAS), which is vital in regulating blood pressure, fluid balance, and electrolyte levels. Here’s a brief overview of how RAAS works:
Renin Release: When blood pressure drops, the kidneys release renin into the bloodstream.
Angiotensinogen Conversion: Renin converts angiotensinogen, a protein produced by the liver, into angiotensin I.
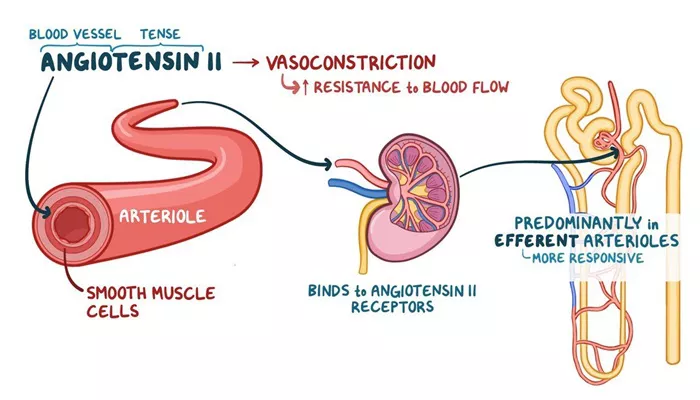
Angiotensin I to Angiotensin II: Angiotensin I is then converted to angiotensin II by the angiotensin-converting enzyme (ACE), primarily in the lungs.
Actions of Angiotensin II: Angiotensin II is a potent vasoconstrictor, meaning it narrows the blood vessels, increasing blood pressure. It also stimulates the release of aldosterone from the adrenal glands, which promotes sodium and water retention by the kidneys, further increasing blood volume and pressure.
In this intricate process, renin’s initial release is crucial. However, when renin levels are abnormally low, it disrupts the balance and functionality of the entire system, potentially leading to hypertension.
Mechanisms by Which Low Renin Levels Cause Hypertension
There are several mechanisms through which low renin levels can lead to hypertension. These mechanisms are often interrelated and can contribute to the overall increase in blood pressure:
Reduced Renin-Angiotensin System Activity
Low renin levels lead to decreased production of angiotensin II. While this might initially seem beneficial, it disrupts the fine-tuned balance of the RAAS. Angiotensin II is responsible for maintaining vascular tone and ensuring adequate blood flow. Insufficient levels can lead to compensatory mechanisms, such as increased sympathetic nervous system activity, which raises blood pressure.
SEE ALSO: How Does Scleroderma Cause Pulmonary Hypertension?
Increased Sodium Retention
Renin deficiency can lead to reduced aldosterone levels. Aldosterone is crucial for sodium and water reabsorption in the kidneys. Low levels of aldosterone cause the kidneys to retain more sodium, increasing blood volume and pressure. This condition is particularly seen in low-renin hypertension, also known as volume-dependent hypertension.
Hyperactivity of the Sympathetic Nervous System
The sympathetic nervous system controls many bodily functions, including heart rate and vascular resistance. In cases of low renin, the body may compensate by increasing sympathetic activity, leading to vasoconstriction and elevated blood pressure. This response can be particularly pronounced in certain forms of secondary hypertension, such as in individuals with adrenal gland disorders.
Altered Vascular Resistance
Chronic low renin levels can lead to changes in the blood vessels themselves. Without adequate angiotensin II, the blood vessels may become less responsive to normal regulatory mechanisms, resulting in increased peripheral resistance. This heightened resistance forces the heart to work harder, raising blood pressure over time.
Conditions Associated with Low Renin Hypertension
Several medical conditions are associated with low renin levels and can contribute to the development of hypertension:
Primary Aldosteronism (Conn’s Syndrome)
Primary aldosteronism is characterized by excessive production of aldosterone by the adrenal glands, independent of renin regulation. The high aldosterone levels lead to increased sodium and water retention, resulting in high blood pressure. Interestingly, despite the high aldosterone, renin levels remain low due to feedback inhibition.
Liddle Syndrome
Liddle syndrome is a rare genetic disorder affecting the sodium channels in the kidneys. These channels become overly active, leading to excessive sodium reabsorption and low renin levels. The resulting hypertension is often severe and resistant to standard treatments.
Chronic Kidney Disease (CKD)
CKD can lead to low renin levels due to damage to the juxtaglomerular cells in the kidneys, which are responsible for renin production. This damage can result from prolonged high blood pressure or other kidney diseases, creating a vicious cycle where low renin exacerbates hypertension, further harming the kidneys.
African-American Hypertension
Studies have shown that African-Americans are more likely to have low renin hypertension compared to other ethnic groups. This form of hypertension often responds better to diuretics and calcium channel blockers rather than RAAS inhibitors.
Diagnosis of Low Renin Hypertension
Diagnosing low renin hypertension involves several steps and tests:
Blood Pressure Measurement
Consistent high blood pressure readings are the initial indicator of hypertension. If standard treatments are ineffective, further investigation into renin levels may be warranted.
Blood Tests
Blood tests can measure plasma renin activity (PRA) and aldosterone levels. Low PRA combined with high aldosterone indicates primary aldosteronism, while low PRA with normal aldosterone suggests other forms of low renin hypertension.
Imaging Studies
Imaging studies, such as CT scans or MRIs, can identify adrenal gland abnormalities, such as tumors, that may be causing excessive aldosterone production.
Genetic Testing
In cases of suspected Liddle syndrome or other genetic conditions, genetic testing can confirm the diagnosis and guide treatment strategies.
Treatment Options for Low Renin Hypertension
Treating low renin hypertension requires a tailored approach, often involving medications and lifestyle changes:
Medications
Diuretics: Diuretics help reduce blood volume by promoting sodium and water excretion, making them effective for volume-dependent hypertension.
Calcium Channel Blockers: These medications relax blood vessels, reducing peripheral resistance and lowering blood pressure.
Mineralocorticoid Receptor Antagonists: Drugs like spironolactone and eplerenone block the effects of aldosterone, reducing sodium retention and lowering blood pressure.
Beta-Blockers: These can be effective in reducing sympathetic nervous system activity, particularly in cases with increased sympathetic tone.
Lifestyle Modifications
Dietary Changes: Reducing sodium intake can significantly impact blood pressure control. A diet rich in fruits, vegetables, and whole grains, such as the DASH diet, is beneficial.
Physical Activity: Regular exercise helps lower blood pressure and improve overall cardiovascular health.
Weight Management: Maintaining a healthy weight reduces the strain on the cardiovascular system and helps control blood pressure.
Conclusion
Low renin hypertension is a complex condition requiring careful diagnosis and management. By understanding the underlying mechanisms and associated conditions, healthcare providers can develop effective treatment plans tailored to each patient’s needs. With proper management, individuals with low renin hypertension can achieve better blood pressure control and reduce their risk of complications. As research continues to uncover more about this subtype of hypertension, new treatment strategies and interventions may emerge, offering hope for even better outcomes in the future.