Re-entry ventricular arrhythmia is a specific type of abnormal heart rhythm originating from the ventricles, the lower chambers of the heart. This condition is characterized by rapid, repetitive electrical impulses that create a circular or re-entrant circuit within the ventricular tissue, leading to a rapid and irregular heartbeat. Understanding re-entry ventricular arrhythmia is crucial for identifying its causes, recognizing its symptoms, and exploring potential treatment options. This article delves into the intricacies of re-entry ventricular arrhythmia, shedding light on its pathophysiology, diagnostic methods, and available therapeutic interventions.
Pathophysiology of Re-Entry Ventricular Arrhythmia
The Mechanism of Re-Entry
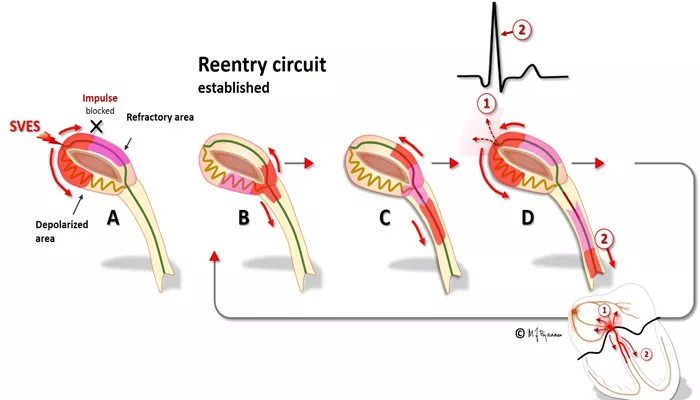
Re-entry ventricular arrhythmia occurs when an electrical impulse travels in a circular path within the ventricular myocardium, leading to continuous and rapid heartbeats. The re-entrant circuit is often established due to differences in the electrical conduction properties of the myocardial tissue. These differences can arise from scar tissue, ischemic areas, or regions with abnormal electrical conduction, creating a pathway for the impulse to re-enter and perpetuate the cycle.
Types of Re-Entry Mechanisms
There are two primary types of re-entry mechanisms: functional and anatomical. Functional re-entry involves areas of slow conduction or refractoriness without any fixed anatomical obstacle, while anatomical re-entry requires a fixed structure, such as scar tissue from a previous myocardial infarction, that forms part of the re-entrant circuit.
Causes And Risk Factors
Underlying Heart Conditions
Re-entry ventricular arrhythmia is commonly associated with underlying heart conditions, particularly those that affect the structural integrity of the ventricles. Myocardial infarction, cardiomyopathy, and heart failure are significant risk factors as they often result in the formation of scar tissue or areas of altered conduction within the myocardium.
SEE ALSO: When Does Arrhythmia Become Dangerous
Genetic Predisposition
Certain genetic conditions can predispose individuals to ventricular arrhythmias. Long QT syndrome, Brugada syndrome, and other inherited channelopathies affect the electrical properties of the heart and increase the likelihood of developing re-entrant circuits.
Electrolyte Imbalances and Medication Effects
Electrolyte imbalances, particularly involving potassium, calcium, and magnesium levels, can disrupt the normal electrical activity of the heart and precipitate arrhythmias. Additionally, certain medications, especially those that affect cardiac conduction, such as antiarrhythmic drugs and some antidepressants, can induce or exacerbate re-entry ventricular arrhythmias.
Symptoms And Clinical Presentation
Palpitations and Tachycardia
The most common symptom of re-entry ventricular arrhythmia is palpitations, where individuals feel an abnormal, rapid, or irregular heartbeat. This sensation is often described as a fluttering or pounding in the chest. Tachycardia, or a heart rate exceeding 100 beats per minute, is typically present during episodes.
Dizziness and Syncope
The rapid and inefficient contraction of the ventricles can lead to reduced cardiac output, causing symptoms of dizziness or lightheadedness. In severe cases, individuals may experience syncope (fainting) due to inadequate blood flow to the brain.
Chest Pain and Shortness of Breath
Chest pain or discomfort, similar to angina, can occur during episodes of re-entry ventricular arrhythmia. Additionally, the compromised cardiac function may lead to shortness of breath, particularly during physical exertion.
Diagnosis
Electrocardiogram (ECG)
An electrocardiogram (ECG) is the primary diagnostic tool for detecting re-entry ventricular arrhythmia. During an episode, the ECG typically shows a rapid and wide QRS complex tachycardia, which is indicative of ventricular origin. The morphology of the QRS complexes can provide clues about the specific type of re-entry mechanism.
Holter Monitoring and Event Recorders
For patients with intermittent symptoms, Holter monitoring or event recorders may be used. These devices continuously record the heart’s electrical activity over an extended period, increasing the likelihood of capturing arrhythmic episodes.
Electrophysiological Study (EPS)
An electrophysiological study (EPS) involves the insertion of catheters into the heart to map the electrical pathways and identify the location of the re-entrant circuit. This invasive procedure is particularly useful for planning catheter ablation, a therapeutic intervention aimed at disrupting the re-entrant pathway.
Treatment Options
Medications
Antiarrhythmic medications are often the first line of treatment for managing re-entry ventricular arrhythmias. Class I and Class III antiarrhythmic drugs, such as flecainide and amiodarone, can help stabilize the heart’s electrical activity and prevent recurrent episodes. Beta-blockers and calcium channel blockers may also be used to control heart rate and reduce symptoms.
Catheter Ablation
Catheter ablation is a minimally invasive procedure that aims to eliminate the re-entrant circuit by delivering radiofrequency energy or cryotherapy to the affected area. This procedure has a high success rate and is often considered for patients with recurrent or refractory arrhythmias.
Implantable Cardioverter-Defibrillator (ICD)
For individuals at high risk of life-threatening arrhythmias, an implantable cardioverter-defibrillator (ICD) may be recommended. This device continuously monitors the heart’s rhythm and delivers electrical shocks to terminate ventricular tachycardia or fibrillation, restoring normal rhythm.
Lifestyle Modifications
Lifestyle changes can play a crucial role in managing re-entry ventricular arrhythmias. Patients are advised to avoid triggers such as excessive caffeine or alcohol intake, manage stress effectively, and adhere to a heart-healthy diet. Regular exercise, under medical supervision, can also improve overall cardiovascular health.
Prognosis And Complications
Prognosis
The prognosis for individuals with re-entry ventricular arrhythmia varies depending on the underlying cause and the effectiveness of treatment. With appropriate management, many patients can achieve good control of their symptoms and maintain a relatively normal quality of life. However, those with severe structural heart disease may have a higher risk of complications.
Complications
Re-entry ventricular arrhythmia can lead to significant complications if not adequately managed. These include heart failure, due to the sustained high heart rates causing the heart to weaken over time, and sudden cardiac death, particularly in patients with severe underlying heart conditions or those who do not receive timely treatment.
Conclusion
Re-entry ventricular arrhythmia is a complex and potentially life-threatening condition characterized by rapid and irregular heartbeats originating from the ventricles. Understanding its pathophysiology, recognizing the symptoms, and seeking appropriate medical intervention are essential steps in managing this arrhythmia effectively. Advances in diagnostic techniques and treatment options, including medications, catheter ablation, and ICDs, have significantly improved the prognosis for many patients.