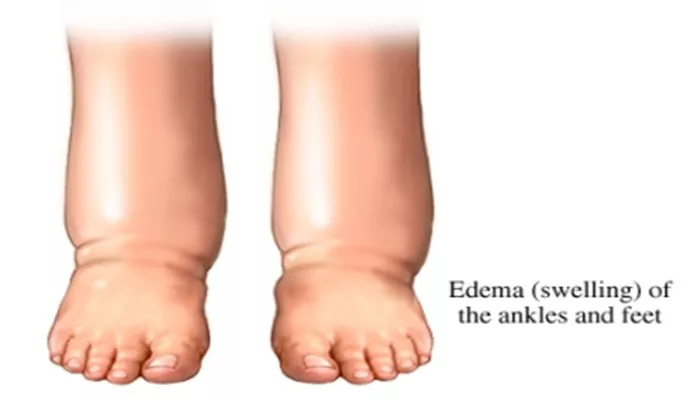
Heart failure is a chronic condition where the heart is unable to pump blood effectively to meet the body’s needs. One of the common complications of heart failure is edema, or swelling, which can occur in various parts of the body, most notably in the legs, ankles, and feet. Understanding the underlying mechanisms that lead to edema in heart failure patients is crucial for effective management and treatment. Here are the eight primary reasons why heart failure can cause edema.
8 Reasons Why Heart Failure Causes Edema
1. Reduced Cardiac Output
Heart failure often results in a reduced cardiac output, which means the heart cannot pump sufficient blood to meet the body’s demands.
This decrease in blood flow can lead to a cascade of physiological responses. When the cardiac output is low, the kidneys receive less blood, which they interpret as dehydration. In response, the kidneys activate mechanisms to retain sodium and water to increase blood volume. This retention of fluid can lead to edema.
2. Increased Venous Pressure
In heart failure, particularly in cases of right-sided heart failure, the heart’s ability to pump blood returning from the body is compromised.
This leads to an increase in venous pressure. When the pressure in the veins is too high, it forces fluid out of the blood vessels and into the surrounding tissues, resulting in edema. This is particularly noticeable in the lower extremities due to the effects of gravity.
see also: The 5 Best Ways to Prevent Heart Failure
3. Activation of the Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a hormone system that regulates blood pressure and fluid balance. When cardiac output is reduced in heart failure, the kidneys activate the RAAS to conserve sodium and water, aiming to increase blood volume and pressure.
However, this compensatory mechanism can backfire, leading to fluid overload and edema. The retention of sodium and water exacerbates the swelling associated with heart failure.
4. Sympathetic Nervous System Activation
Heart failure triggers the activation of the sympathetic nervous system, which increases heart rate and constricts blood vessels to maintain blood pressure and perfusion. However, chronic activation of this system can lead to vasoconstriction, increased afterload (resistance the heart must pump against), and further reduction in cardiac output.
Additionally, this sympathetic activation promotes the release of hormones that cause the kidneys to retain sodium and water, contributing to edema.
5. Capillary Fluid Shift
The capillaries are small blood vessels where the exchange of oxygen, nutrients, and waste products occurs between the blood and tissues.
In heart failure, the pressure within these capillaries can increase due to elevated venous pressure and reduced cardiac output. This elevated pressure forces fluid out of the capillaries and into the interstitial spaces (the space between cells), leading to edema.
6. Lymphatic System Overload
The lymphatic system is responsible for returning excess fluid from tissues back into the bloodstream. In heart failure, the increased fluid retention and elevated venous pressures can overwhelm the lymphatic system’s capacity to return this fluid.
When the lymphatic system is overloaded, fluid accumulates in the tissues, causing edema.
7. Decreased Oncotic Pressure
Oncotic pressure is the pressure exerted by proteins, primarily albumin, in the blood plasma that pulls fluid into the bloodstream from the surrounding tissues. In heart failure, there may be a reduction in the production of these proteins or an increased loss of proteins through the kidneys (proteinuria). Reduced oncotic pressure allows fluid to leak out of the blood vessels and into the surrounding tissues, contributing to edema.
8. Medication Side Effects
Many medications used to treat heart failure can have side effects that contribute to edema. For example, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and certain blood pressure medications can cause sodium and water retention. Additionally, some heart failure patients may be on medications that dilate blood vessels, which can also lead to fluid leakage into the tissues. It is important to manage these medications carefully to balance the benefits of treatment with the risk of exacerbating edema.
Conclusion
Edema in heart failure is a multifactorial condition arising from the complex interplay of various physiological mechanisms.
Reduced cardiac output, increased venous pressure, activation of the RAAS and sympathetic nervous system, capillary fluid shift, lymphatic system overload, decreased oncotic pressure, and medication side effects all contribute to the development of edema in heart failure patients. Understanding these mechanisms is essential for healthcare providers to effectively manage and treat edema in individuals with heart failure, improving their quality of life and clinical outcomes.
Managing edema in heart failure typically involves a combination of lifestyle changes, medication adjustments, and in some cases, more advanced interventions. Patients are often advised to reduce their sodium intake, maintain a healthy weight, and follow prescribed medication regimens carefully. Diuretics are commonly used to help the body expel excess fluid, and other medications may be adjusted to optimize heart function and minimize fluid retention. Regular follow-up with a healthcare provider is crucial to monitor the condition and adjust treatment as necessary.