Coronary artery disease (CAD), also known as ischemic heart disease, is one of the leading causes of morbidity and mortality worldwide. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to atherosclerosis—the buildup of plaques composed of fat, cholesterol, and other substances. Early diagnosis and management of CAD are crucial for preventing serious complications such as myocardial infarction (heart attack) and heart failure. This article delves into the methods used to diagnose CAD and identifies the groups of people who should be screened and monitored closely.
Signs And Symptoms of Coronary Artery Disease
CAD can be asymptomatic in its early stages. As the disease progresses, symptoms may include:
Angina Pectoris: This is chest pain or discomfort that occurs when the heart muscle doesn’t get enough oxygen-rich blood.
It often feels like pressure or squeezing in the chest and may radiate to the shoulders, arms, neck, jaw, or back.
Shortness of Breath: This can occur with exertion or at rest and may be accompanied by fatigue.
Heart Attack: Severe chest pain, shortness of breath, nausea, and sweating may indicate a heart attack, which is a medical emergency.
Recognizing these symptoms is essential for timely diagnosis and intervention.
SEE ALSO: What Are The Seven Dietary Factors of Coronary Heart Disease
Risk Factors for Coronary Artery Disease
Certain groups of people are at higher risk for developing CAD and should be closely monitored. Risk factors include:
Age: Risk increases with age, especially for men over 45 and women over 55.
Gender: Men are at higher risk than pre-menopausal women. After menopause, the risk for women increases.
Family History: A family history of heart disease increases risk.
Smoking: Tobacco use significantly raises the risk of CAD.
High Blood Pressure: Hypertension damages arteries, making them more susceptible to atherosclerosis.
High Cholesterol: Elevated levels of LDL (bad) cholesterol contribute to plaque formation.
Diabetes: Diabetes increases the risk of CAD due to associated high blood sugar levels.
Obesity: Excess weight strains the heart and promotes atherosclerosis.
Physical Inactivity: Lack of exercise contributes to many risk factors, including obesity and high blood pressure.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, and sodium contribute to the development of CAD.
Stress: Chronic stress may damage arteries and worsen other risk factors.
Diagnostic Methods for Coronary Artery Disease
1. Medical History and Physical Examination
The diagnostic process begins with a thorough medical history and physical examination. The physician will inquire about the patient’s symptoms, risk factors, family history of heart disease, and lifestyle habits. During the physical exam, the doctor will check for signs of cardiovascular problems, such as abnormal heart sounds or swelling in the legs.
2. Electrocardiogram (ECG or EKG)
An electrocardiogram is a non-invasive test that records the electrical activity of the heart. It can detect:
Arrhythmias: Irregular heart rhythms that may indicate heart problems.
Ischemia: Reduced blood flow to the heart muscle.
Myocardial Infarction: Evidence of a previous heart attack.
While an ECG can provide important information, it may not detect all cases of CAD, especially if the patient is not experiencing symptoms at the time of the test.
3. Stress Testing
Stress testing evaluates how the heart performs under physical stress.
There are several types of stress tests:
Exercise Stress Test: The patient exercises on a treadmill or stationary bike while their heart rate, blood pressure, and ECG are monitored. This test can reveal signs of ischemia that may not be apparent at rest.
Pharmacological Stress Test: For patients unable to exercise, medications such as adenosine, dipyridamole, or dobutamine are used to simulate the effects of exercise on the heart.
Stress tests can help determine the severity of CAD and guide treatment decisions.
4. Echocardiogram
An echocardiogram uses ultrasound waves to create images of the heart’s structures and assess its function. It can provide information about:
Heart Chambers and Valves: Size and function.
Blood Flow: Through the heart and major vessels.
Wall Motion Abnormalities: Areas of the heart muscle that are not contracting properly, which may indicate ischemia or previous heart damage.
5. Nuclear Cardiology Imaging
Nuclear imaging techniques, such as myocardial perfusion imaging (MPI), involve the use of radioactive tracers to visualize blood flow to the heart muscle. These tests can detect areas of reduced blood flow and assess the extent of CAD. Common nuclear imaging tests include:
Single Photon Emission Computed Tomography (SPECT): Provides detailed images of blood flow to the heart.
Positron Emission Tomography (PET): Offers higher resolution images and can quantify blood flow.
6. Coronary Angiography
Coronary angiography is considered the gold standard for diagnosing CAD. This invasive procedure involves:
Catheter Insertion: A catheter is inserted into a blood vessel, usually in the groin or wrist, and guided to the coronary arteries.
Contrast Dye Injection: A contrast dye is injected through the catheter to visualize the coronary arteries on X-ray images.
Coronary angiography can identify the location and severity of arterial blockages and guide decisions about interventions such as angioplasty or coronary artery bypass surgery.
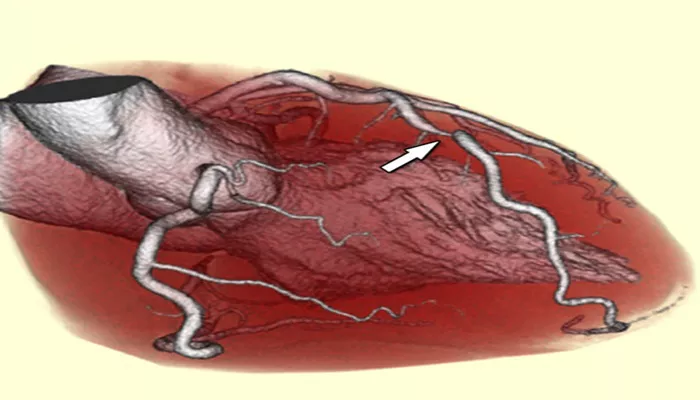
7. Computed Tomography Angiography (CTA)
CTA is a non-invasive imaging technique that uses CT scanning and contrast dye to visualize the coronary arteries. It provides detailed images and can detect:
Plaque Buildup: The presence of atherosclerotic plaques.
Narrowing of Arteries: The degree of stenosis.
CTA is particularly useful for patients with an intermediate risk of CAD and can help rule out the disease in symptomatic patients.
8. Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI uses powerful magnets and radio waves to create detailed images of the heart and blood vessels. It can assess:
Heart Structure and Function: Including wall motion and valve function.
Myocardial Perfusion: Blood flow to the heart muscle.
Tissue Characterization: Identifying scar tissue or inflammation.
Cardiac MRI is valuable for evaluating complex cases and assessing the extent of heart damage.
Conclusion
Early diagnosis of coronary artery disease is crucial for preventing serious cardiovascular events and improving patient outcomes. A combination of medical history, physical examination, and various diagnostic tests can effectively identify CAD and guide appropriate management. Regular screening and monitoring of high-risk individuals can help detect the disease in its early stages, allowing for timely intervention and better prognosis.