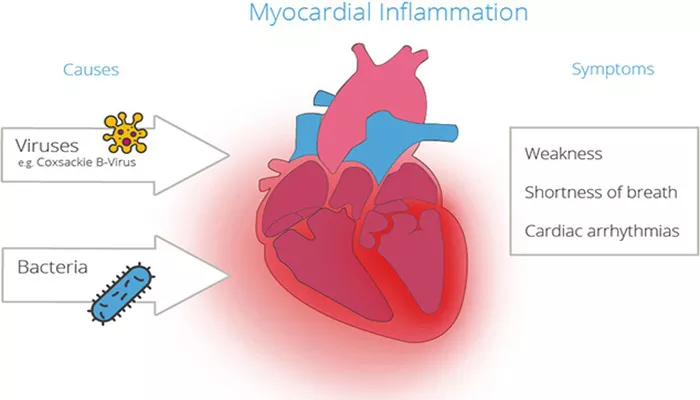
Myocarditis is a condition characterized by inflammation of the myocardium, the middle layer of the heart wall. This inflammation can weaken the heart, reduce its ability to pump blood, and cause rapid or abnormal heart rhythms.
Understanding myocarditis is crucial as it can have serious implications for heart health and overall well-being.
Definition And Causes of Myocarditis
Myocarditis refers to the inflammation of the heart muscle, which can result from various infectious and non-infectious causes. The inflammation can impair the heart’s electrical system, leading to arrhythmias, or reduce the heart’s ability to pump blood effectively, potentially causing heart failure.
Infectious Causes
Viral Infections:
Coxsackievirus B: This virus is one of the most common causes of myocarditis. It often affects children and young adults.
Adenovirus: Another frequent cause, adenovirus can lead to respiratory infections that sometimes spread to the heart.
Herpesviruses: These include Epstein-Barr virus (EBV) and cytomegalovirus (CMV), which can cause myocarditis, particularly in immunocompromised individuals.
Bacterial Infections:
Streptococcus and Staphylococcus: These bacteria can lead to myocarditis, often following a severe bacterial infection such as pneumonia or a skin infection.
Mycobacterium: The bacteria responsible for tuberculosis can also cause myocarditis, particularly in areas where TB is prevalent.
SEE ALSO: How Is Myocarditis Transmitted?
Fungal Infections:
Candida and Aspergillus: These fungi can cause myocarditis, primarily in individuals with weakened immune systems.
Parasitic Infections:
Trypanosoma cruzi: The parasite responsible for Chagas disease, common in Latin America, is a significant cause of myocarditis.
Toxoplasma gondii: This parasite, often contracted from undercooked meat or cat feces, can cause myocarditis, especially in immunocompromised individuals.
Non-Infectious Causes
Autoimmune Diseases:
Lupus and Rheumatoid Arthritis: These conditions can lead to inflammation of various organs, including the heart.
Giant Cell Myocarditis: A rare but severe form of myocarditis often associated with autoimmune conditions.
Medications and Toxins:
Certain Chemotherapy Drugs: Medications used to treat cancer can sometimes cause myocarditis.
Cocaine and Alcohol: These substances can lead to myocarditis through direct toxic effects on the heart muscle.
Allergic Reactions:
Drug Allergies: Severe allergic reactions to medications can sometimes involve the heart, leading to myocarditis.
Symptoms And Diagnosis
Symptoms
The symptoms of myocarditis can vary widely, from mild to severe, and may mimic other heart conditions. Common symptoms include:
Chest Pain: This can be sharp or stabbing, and it may increase with deep breaths or physical activity.
Shortness of Breath: This may occur at rest or with exertion and can be a sign of heart failure.
Fatigue: Generalized tiredness and weakness are common.
Heart Palpitations: Rapid or irregular heartbeats can occur.
Flu-like Symptoms: Fever, body aches, and sore throat often accompany viral myocarditis.
Swelling: In the legs, ankles, and feet due to fluid retention.
Syncope: Fainting or light-headedness, particularly during physical activity.
Diagnosis
Diagnosing myocarditis involves a combination of medical history, physical examination, and diagnostic tests:
Electrocardiogram (ECG): To detect abnormalities in the heart’s electrical activity.
Echocardiogram: An ultrasound of the heart to assess its structure and function.
Cardiac MRI: This imaging test provides detailed pictures of the heart’s structure and can identify areas of inflammation.
Blood Tests: To check for markers of inflammation and infection.
Endomyocardial Biopsy: A procedure where a small sample of heart tissue is taken and examined under a microscope to confirm the diagnosis.
Treatment of Myocarditis
General Measures
Rest: Reducing physical activity can help decrease the strain on the heart.
Fluid and Salt Restriction: To manage symptoms of heart failure and fluid retention.
Medications
Anti-inflammatory Drugs: To reduce inflammation and pain.
NSAIDs: Non-steroidal anti-inflammatory drugs can be used, although their use is controversial due to potential adverse effects on heart function.
Corticosteroids: These may be prescribed in severe cases or when myocarditis is caused by autoimmune conditions.
Heart Medications:
ACE Inhibitors and ARBs: To reduce blood pressure and ease the heart’s workload.
Beta-blockers: To control heart rate and prevent arrhythmias.
Diuretics: To manage fluid retention and swelling.
Antiviral or Antimicrobial Therapy: If a specific infectious agent is identified, targeted therapy may be necessary.
Advanced Treatments
Intravenous Immunoglobulin (IVIG): Used in some cases to modulate the immune response.
Mechanical Support: In severe cases, devices like ventricular assist devices (VADs) or extracorporeal membrane oxygenation (ECMO) may be necessary to support heart function.
Heart Transplant: In cases of refractory heart failure, a heart transplant may be considered.
Conclusion
Myocarditis is a complex condition with a variety of causes, symptoms, and outcomes. Early recognition and appropriate treatment are crucial for managing the disease and preventing long-term complications. Individuals at higher risk should be particularly vigilant and take preventive measures to protect their heart health. Understanding myocarditis can help in making informed decisions about health and well-being, ultimately leading to better outcomes for those affected by this condition.