Hyperlipidemia, often referred to as high cholesterol, is a condition characterized by elevated levels of lipids (fats) in the blood. These lipids include cholesterol and triglycerides, which are essential for various bodily functions but can lead to health problems when present in excessive amounts. Hyperlipidemia is a significant risk factor for cardiovascular diseases, including heart attack and stroke. Early detection and management are crucial for preventing these complications, and laboratory tests play a vital role in diagnosing hyperlipidemia.
Key Lipids In The Blood
Before delving into the specific laboratory tests, it is important to understand the different types of lipids measured:
Total Cholesterol: This is the overall amount of cholesterol in the blood, including both low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
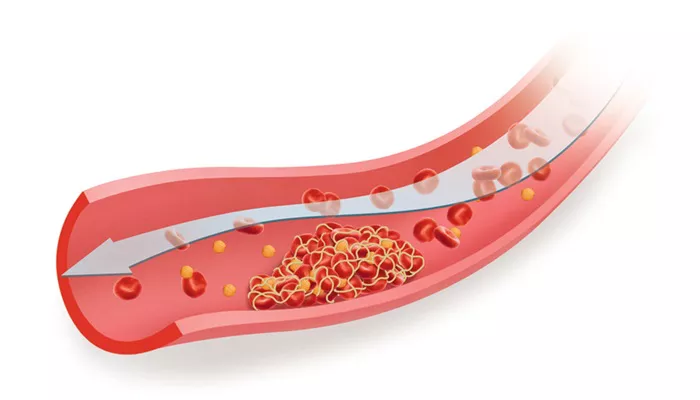
Low-Density Lipoprotein (LDL) Cholesterol: Often called “bad” cholesterol, LDL cholesterol can accumulate in the walls of arteries, leading to atherosclerosis, which increases the risk of heart disease and stroke.
High-Density Lipoprotein (HDL) Cholesterol: Known as “good” cholesterol, HDL cholesterol helps remove excess cholesterol from the bloodstream, transporting it to the liver for excretion.
Triglycerides: These are the most common type of fat in the body, stored in fat cells and used for energy. High levels of triglycerides can also contribute to atherosclerosis.
Very Low-Density Lipoprotein (VLDL) Cholesterol: VLDL carries triglycerides in the blood. Like LDL, high levels of VLDL can contribute to plaque buildup in the arteries.
SEE ALSO: The 7 Best Ways to Reduce Hyperlipidemia
Laboratory Tests for Hyperlipidemia
Lipid Panel
The primary laboratory test used to diagnose hyperlipidemia is the lipid panel, also known as a lipid profile. This test measures the levels of various lipids in the blood, providing a comprehensive picture of a person’s lipid status. The lipid panel typically includes:
- Total Cholesterol
- LDL Cholesterol
- HDL Cholesterol
- Triglycerides
Fasting Lipid Panel
A fasting lipid panel requires the patient to fast (refrain from eating or drinking anything except water) for 9-12 hours before the blood sample is taken. Fasting helps ensure accurate measurements, particularly of triglycerides and LDL cholesterol. The results of a fasting lipid panel are interpreted as follows:
Total Cholesterol:
- Desirable: Less than 200 mg/dL
- Borderline High: 200-239 mg/dL
- High: 240 mg/dL and above
LDL Cholesterol:
- Optimal: Less than 100 mg/dL
- Near Optimal: 100-129 mg/dL
- Borderline High: 130-159 mg/dL
- High: 160-189 mg/dL
- Very High: 190 mg/dL and above
HDL Cholesterol:
Low (Risk Factor for Heart Disease): Less than 40 mg/dL for men, Less than 50 mg/dL for women
Optimal: 60 mg/dL and above
Triglycerides:
- Normal: Less than 150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: 500 mg/dL and above
Non-Fasting Lipid Panel
Recent guidelines suggest that non-fasting lipid panels can also be used to assess lipid levels, particularly in individuals without a history of hyperlipidemia or cardiovascular disease. While triglyceride levels may be slightly higher in a non-fasting state, the overall lipid profile remains a valuable diagnostic tool.
Apolipoprotein Measurements
Apolipoproteins are the protein components of lipoproteins, which transport lipids in the blood. Measuring apolipoproteins can provide additional information about lipid metabolism and cardiovascular risk:
Apolipoprotein B (ApoB): ApoB is the primary protein found in LDL and VLDL particles. Elevated ApoB levels are associated with an increased risk of cardiovascular disease, as they reflect the number of atherogenic particles in the blood.
Apolipoprotein A1 (ApoA1): ApoA1 is the main protein component of HDL particles. Higher levels of ApoA1 are typically associated with a lower risk of cardiovascular disease.
Lipoprotein(a) [Lp(a)]
Lipoprotein(a) is a type of lipoprotein similar to LDL but with an additional protein called apolipoprotein(a). Elevated Lp(a) levels are an independent risk factor for cardiovascular disease, particularly in individuals with a family history of early heart disease. Lp(a) levels are primarily determined by genetics and are less influenced by lifestyle factors.
High-Sensitivity C-Reactive Protein (hs-CRP)
Although not a lipid, high-sensitivity C-reactive protein (hs-CRP) is an inflammatory marker that can be measured alongside lipid levels to assess cardiovascular risk. Elevated hs-CRP levels indicate increased inflammation, which is associated with a higher risk of atherosclerosis and cardiovascular events. When used in conjunction with lipid panels, hs-CRP can provide a more comprehensive assessment of cardiovascular risk.
Genetic Testing
In some cases, genetic testing may be recommended to identify specific genetic mutations associated with hyperlipidemia.
Conditions such as familial hypercholesterolemia (FH) are caused by genetic mutations that lead to significantly elevated LDL cholesterol levels and an increased risk of early cardiovascular disease. Identifying these genetic mutations can help guide treatment and management strategies.
Interpreting Laboratory Results
Interpreting laboratory results for hyperlipidemia involves comparing the measured lipid levels to established reference ranges and guidelines. Healthcare providers consider several factors when assessing a patient’s lipid profile:
Age and Gender: Lipid levels can vary based on age and gender, with men generally having higher total cholesterol and LDL cholesterol levels than women before menopause.
Family History: A family history of hyperlipidemia or cardiovascular disease can indicate a genetic predisposition to elevated lipid levels.
Lifestyle Factors: Diet, physical activity, smoking, and alcohol consumption can all influence lipid levels. Healthcare providers assess these factors to determine the potential impact on lipid levels.
Underlying Health Conditions: Conditions such as diabetes, hypothyroidism, and kidney disease can affect lipid metabolism and contribute to hyperlipidemia.
Medications: Certain medications, including statins, fibrates, and bile acid sequestrants, are used to manage hyperlipidemia. The effectiveness of these medications is monitored through regular lipid panel testing.
Management of Hyperlipidemia
The management of hyperlipidemia typically involves a combination of lifestyle modifications and pharmacotherapy:
Lifestyle Modifications
Dietary Changes:
Reduce intake of saturated and trans fats.
Increase consumption of fruits, vegetables, whole grains, and lean proteins.
Incorporate healthy fats from sources such as olive oil, nuts, and fatty fish.
Physical Activity:
Engage in regular aerobic exercise (e.g., brisk walking, running, cycling) for at least 150 minutes per week.
Include strength training exercises at least twice a week.
Weight Management:
Achieve and maintain a healthy weight through a combination of diet and exercise.
Smoking Cessation:
Quit smoking to improve HDL cholesterol levels and overall cardiovascular health.
Alcohol Moderation:
Limit alcohol consumption to moderate levels (up to one drink per day for women and up to two drinks per day for men).
Pharmacotherapy
For individuals who cannot achieve optimal lipid levels through lifestyle modifications alone, medications may be prescribed:
Statins: Statins are the first-line treatment for lowering LDL cholesterol levels and reducing cardiovascular risk. They work by inhibiting an enzyme involved in cholesterol synthesis in the liver.
Fibrates: Fibrates are used to lower triglyceride levels and increase HDL cholesterol levels. They are particularly effective in individuals with high triglycerides.
Bile Acid Sequestrants: These medications bind to bile acids in the intestine, preventing their reabsorption and promoting the excretion of cholesterol.
Cholesterol Absorption Inhibitors: Ezetimibe is a medication that reduces the absorption of cholesterol from the intestine, lowering LDL cholesterol levels.
PCSK9 Inhibitors: These injectable medications target a protein called PCSK9, which affects LDL receptor function. By inhibiting PCSK9, these medications can significantly lower LDL cholesterol levels.
Omega-3 Fatty Acids: Prescription-strength omega-3 fatty acid supplements can help lower triglyceride levels.
Niacin: Niacin (vitamin B3) can raise HDL cholesterol levels and lower triglycerides, although its use has decreased due to potential side effects.
Conclusion
Hyperlipidemia is a common and significant risk factor for cardiovascular disease. Laboratory tests, particularly the lipid panel, are essential for diagnosing and monitoring this condition. By understanding and interpreting these tests, healthcare providers can develop effective management plans that include lifestyle modifications and pharmacotherapy to reduce lipid levels and mitigate cardiovascular risk.