Supraventricular Tachycardia (SVT) is a type of arrhythmia, or irregular heartbeat, that originates above the heart’s ventricles. It is characterized by an abnormally fast heart rate, typically over 100 beats per minute, which can sometimes reach upwards of 250 beats per minute. SVT is a common heart condition that can affect individuals of all ages, from infants to the elderly. While it is generally not life-threatening, it can cause significant discomfort and impact the quality of life.
This article delves into the intricacies of SVT, exploring its types, causes, symptoms, diagnosis, and treatment options.
Types of SVT
SVT is an umbrella term that encompasses several different types of arrhythmias. The most common types include:
1. Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
AVNRT is the most prevalent form of SVT, accounting for about 60% of all cases. It occurs when there is a reentrant circuit within or near the atrioventricular (AV) node, leading to rapid and regular heartbeats.
2. Atrioventricular Reentrant Tachycardia (AVRT)
AVRT involves an extra pathway that connects the atria and ventricles, bypassing the AV node. This extra pathway allows electrical impulses to loop back to the atria, causing rapid heartbeats. A common form of AVRT is Wolff-Parkinson-White (WPW) syndrome.
see also: Who Is Most Likely to Get Arrhythmia?
3. Atrial Tachycardia
Atrial Tachycardia arises from abnormal electrical signals in the atria, leading to an abnormally fast heart rate. Unlike AVNRT and AVRT, atrial tachycardia does not involve reentrant circuits.
4. Paroxysmal Supraventricular Tachycardia (PSVT)
PSVT refers to episodes of SVT that start and stop suddenly. These episodes can last from a few seconds to several hours and may occur sporadically.
Causes of SVT
The exact cause of SVT is often unknown, but several factors can contribute to its development:
1. Electrophysiological Abnormalities
Abnormal electrical pathways or circuits in the heart can predispose individuals to SVT. These abnormalities can be congenital or develop over time.
2. Heart Disease
Conditions such as coronary artery disease, heart failure, and cardiomyopathy can increase the risk of SVT. Structural heart abnormalities can also play a role.
3. Lifestyle Factors
Certain lifestyle factors, including excessive caffeine or alcohol consumption, smoking, and stress, can trigger SVT episodes.
4. Medications
Some medications, particularly those that affect the heart’s electrical system, can induce SVT. These include stimulants, decongestants, and certain antidepressants.
5. Medical Conditions
Other medical conditions, such as hyperthyroidism and electrolyte imbalances, can contribute to the development of SVT.
Symptoms of SVT
The symptoms of SVT can vary in severity and may include:
Palpitations
A sensation of a rapid, fluttering, or pounding heartbeat is one of the most common symptoms of SVT.
Dizziness or Lightheadedness
The rapid heart rate can reduce blood flow to the brain, causing dizziness or lightheadedness.
Shortness of Breath
Some individuals with SVT may experience difficulty breathing or a feeling of breathlessness.
Chest Pain or Discomfort
Chest pain or discomfort, often described as a tightness or pressure, can occur during an SVT episode.
Fatigue
The heart’s increased workload during SVT can lead to fatigue or a general feeling of weakness.
Anxiety
The sudden onset of rapid heartbeats can cause anxiety or panic in some individuals.
Diagnosis of SVT
Diagnosing SVT typically involves a combination of medical history, physical examination, and diagnostic tests:
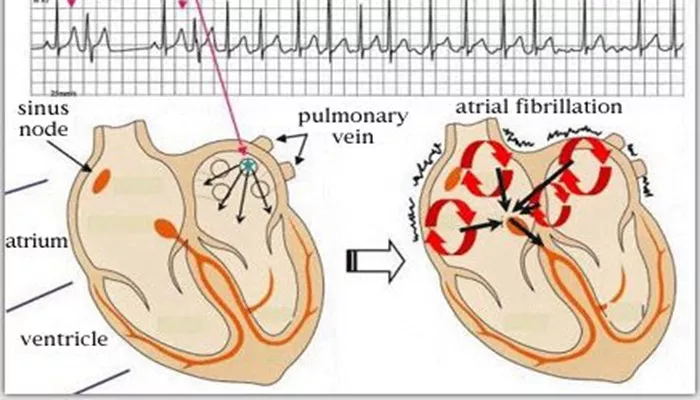
Electrocardiogram (ECG)
An ECG records the electrical activity of the heart and can help identify abnormal rhythms associated with SVT. During an SVT episode, the ECG can reveal a rapid heart rate with narrow QRS complexes.
Holter Monitor
A Holter monitor is a portable ECG device worn for 24 to 48 hours to record the heart’s activity over an extended period. It is useful for detecting intermittent SVT episodes.
Event Monitor
Similar to a Holter monitor, an event monitor is used for longer periods, typically up to a month. It records heart activity when the patient experiences symptoms and activates the device.
Electrophysiological Study (EPS)
An EPS involves threading catheters through blood vessels to the heart to map its electrical activity. This invasive test can help pinpoint the location of abnormal pathways and guide treatment.
Echocardiogram
An echocardiogram uses ultrasound to create images of the heart’s structure and function. It can help identify underlying heart conditions that may contribute to SVT.
Treatment Options for SVT
Treatment for SVT aims to control episodes, alleviate symptoms, and prevent recurrence. The choice of treatment depends on the type and severity of SVT, as well as the patient’s overall health. Common treatment options include:
Vagal Maneuvers
Vagal maneuvers are simple techniques that can help slow down the heart rate by stimulating the vagus nerve. These include:
Valsalva Maneuver: Bearing down as if having a bowel movement.
Carotid Sinus Massage: Gently massaging the carotid artery in the neck.
Diving Reflex: Immersing the face in cold water.
Medications
Several medications can help manage SVT:
Beta-Blockers: These drugs reduce heart rate and decrease the likelihood of SVT episodes.
Calcium Channel Blockers: These medications help slow the heart rate and prevent SVT.
Antiarrhythmic Drugs: These drugs, such as flecainide or propafenone, help restore and maintain a normal heart rhythm.
Catheter Ablation
Catheter ablation is a minimally invasive procedure that involves threading catheters through blood vessels to the heart.
Radiofrequency energy or cryotherapy is used to destroy the abnormal pathways causing SVT. This procedure has a high success rate and is often considered when medications are ineffective or not tolerated.
Electrical Cardioversion
In some cases, electrical cardioversion may be necessary to restore a normal heart rhythm. This procedure involves delivering a controlled electrical shock to the heart.
Lifestyle Modifications
Making lifestyle changes can help reduce the frequency and severity of SVT episodes:
Avoiding Triggers: Identifying and avoiding triggers such as caffeine, alcohol, and stress.
Regular Exercise: Engaging in regular physical activity to improve overall heart health.
Healthy Diet: Maintaining a balanced diet low in sodium and high in fruits, vegetables, and whole grains.
Living with SVT
Living with SVT can be challenging, but with proper management and support, individuals can lead healthy and fulfilling lives. Here are some tips for managing SVT:
Education and Awareness
Understanding the condition and recognizing the symptoms can help individuals manage SVT more effectively. Education about the triggers and management strategies is crucial.
Regular Medical Follow-Up
Regular check-ups with a healthcare provider are essential to monitor the condition and adjust treatment as needed.
Support Networks
Connecting with support groups or online communities can provide emotional support and practical advice from others living with SVT.
Emergency Plan
Having an emergency plan in place, including knowing when to seek medical help, can provide peace of mind.
Conclusion
Supraventricular Tachycardia (SVT) is a common type of arrhythmia that can significantly impact an individual’s quality of life. While it can be distressing, SVT is generally not life-threatening and can be effectively managed with a combination of lifestyle modifications, medications, and medical procedures. Understanding the condition, recognizing the symptoms, and working closely with healthcare providers are key to managing SVT and maintaining a healthy, active lifestyle.