Calcium channel blockers (CCBs) are a class of medications widely used to treat various cardiovascular conditions, including hypertension and angina. However, their use in heart failure requires careful consideration due to potential adverse effects on cardiac function. This article delves into which CCBs should be avoided in heart failure, the underlying mechanisms, and the clinical evidence supporting these recommendations.
Understanding Heart Failure And CCBs
Heart failure is a complex syndrome characterized by the heart’s inability to pump blood effectively, leading to symptoms such as shortness of breath, fatigue, and fluid retention. The pathophysiology of heart failure involves impaired myocardial contractility, increased ventricular stiffness, and neurohormonal activation.
CCBs function by inhibiting the influx of calcium ions into cardiac and smooth muscle cells, leading to vasodilation and reduced myocardial oxygen demand. They are divided into two main classes:
Dihydropyridines (e.g., amlodipine, nifedipine): Primarily act on vascular smooth muscle, causing vasodilation.
Non-dihydropyridines (e.g., verapamil, diltiazem): Affect both the heart and vascular smooth muscle, reducing heart rate and myocardial contractility.
CCBs to Avoid in Heart Failure
1. Non-Dihydropyridine CCBs
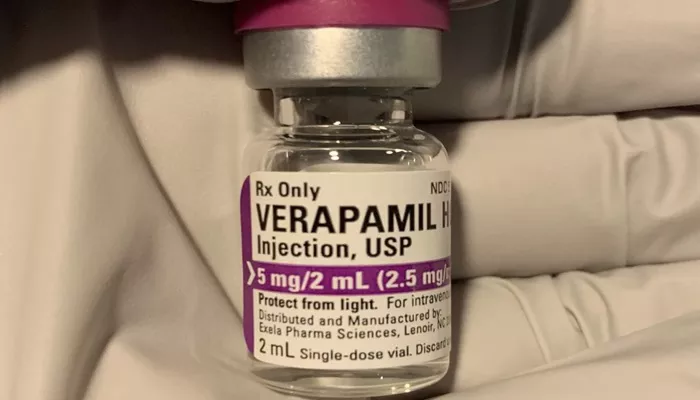
Verapamil and Diltiazem
Verapamil and diltiazem are non-dihydropyridine CCBs that can negatively impact heart failure due to their effects on myocardial contractility and heart rate. They decrease the force of myocardial contraction (negative inotropic effect) and slow the heart rate (negative chronotropic effect), which can exacerbate heart failure symptoms and worsen outcomes.
Clinical Evidence
Verapamil: Studies have shown that verapamil can worsen heart failure symptoms and increase hospitalization rates in patients with left ventricular dysfunction. The negative inotropic effect of verapamil can lead to a further decline in cardiac output in heart failure patients.
Diltiazem: Similar to verapamil, diltiazem’s negative inotropic and chronotropic effects can lead to the decompensation of heart failure. Clinical trials have indicated that diltiazem can worsen symptoms and reduce exercise tolerance in patients with heart failure.
SEE ALSO: The 5 Best Ways to Prevent Heart Failure
Mechanisms of Harm
Negative Inotropic Effect: Both verapamil and diltiazem reduce the contractile force of the heart, which can significantly decrease cardiac output in patients with already compromised heart function.
Bradycardia: By slowing the heart rate, these medications can reduce cardiac output, further compromising the hemodynamic status of heart failure patients.
Conduction Delays: Verapamil and diltiazem can exacerbate conduction abnormalities, leading to arrhythmias that can further deteriorate cardiac function.
2. Dihydropyridine CCBs
While dihydropyridine CCBs are generally considered safer in heart failure compared to non-dihydropyridines, certain agents within this class can still pose risks, especially in high doses or specific clinical scenarios.
3. Nifedipine (Immediate-Release)
Nifedipine, particularly in its immediate-release form, should be avoided in heart failure due to its potential to cause reflex tachycardia and exacerbate myocardial ischemia.
Clinical Evidence
Nifedipine IR: Immediate-release nifedipine has been associated with increased mortality and morbidity in heart failure patients. Its rapid onset and short duration can lead to fluctuations in blood pressure, precipitating reflex tachycardia, which can increase myocardial oxygen demand and worsen heart failure symptoms.
Mechanisms of Harm
Reflex Tachycardia: The sudden vasodilation caused by immediate-release nifedipine can trigger reflex tachycardia, which increases myocardial oxygen consumption and can precipitate ischemia in heart failure patients.
Hypotension: Rapid blood pressure reduction can lead to hypotension, reducing perfusion to vital organs and exacerbating heart failure symptoms.
CCBs with Cautionary Use
Amlodipine
Amlodipine, a dihydropyridine CCB, has been studied in heart failure with more favorable outcomes compared to other CCBs. However, caution is still warranted.
Clinical Evidence
Amlodipine: The PRAISE (Prospective Randomized Amlodipine Survival Evaluation) study demonstrated that amlodipine did not significantly increase mortality in patients with heart failure and may have some beneficial effects in specific subgroups, such as those with non-ischemic cardiomyopathy.
Mechanisms of Benefit
Vasodilation: Amlodipine primarily acts on vascular smooth muscle, causing vasodilation and reducing afterload, which can be beneficial in heart failure.
Minimal Negative Inotropic Effect: Unlike verapamil and diltiazem, amlodipine has minimal negative inotropic effects, making it safer for use in heart failure.
Conclusion
In conclusion, the use of CCBs in heart failure requires careful selection and monitoring. Non-dihydropyridine CCBs such as verapamil and diltiazem should be avoided due to their negative inotropic and chronotropic effects, which can worsen heart failure outcomes. Immediate-release nifedipine is also contraindicated due to its potential to cause reflex tachycardia and hypotension.
Dihydropyridine CCBs like amlodipine may be used with caution in heart failure, particularly in patients with hypertension or angina who require additional management. However, the decision to use any CCB in heart failure should be individualized, taking into account the patient’s overall clinical status and concomitant conditions.