Insulin resistance and hyperlipidemia are two interconnected metabolic conditions that significantly impact public health.
Insulin resistance is a state in which the body’s cells become less responsive to the hormone insulin, leading to elevated blood glucose levels. Hyperlipidemia, on the other hand, refers to abnormally high levels of lipids (fats) in the blood, which include cholesterol and triglycerides. The relationship between these two conditions is complex and multifaceted, and understanding how insulin resistance causes hyperlipidemia can provide insights into the prevention and management of metabolic disorders.
The Role of Insulin in Metabolism
Insulin is a hormone produced by the pancreas that plays a crucial role in regulating metabolism. Its primary functions include:
Glucose Uptake: Insulin facilitates the uptake of glucose by cells, particularly in the liver, muscle, and adipose tissue, where it is used for energy or stored as glycogen.
Lipid Metabolism: Insulin inhibits the breakdown of fats (lipolysis) in adipose tissue and promotes the synthesis of fatty acids and triglycerides in the liver.
Protein Synthesis: Insulin supports the synthesis of proteins by promoting the uptake of amino acids into cells.
When insulin function is impaired, as in insulin resistance, these metabolic processes are disrupted, leading to a cascade of metabolic disturbances.
Mechanisms Linking Insulin Resistance to Hyperlipidemia
1. Increased Free Fatty Acid Release
In insulin resistance, the body’s cells do not respond effectively to insulin, leading to decreased glucose uptake. This results in elevated blood glucose levels, prompting the pancreas to secrete more insulin.
Despite the increased insulin levels, the resistance continues, creating a vicious cycle.
In adipose tissue, insulin normally inhibits the breakdown of stored triglycerides into free fatty acids (FFAs). However, in insulin-resistant states, this inhibition is impaired, leading to increased lipolysis and the release of FFAs into the bloodstream. Elevated FFAs contribute to the development of hyperlipidemia in several ways:
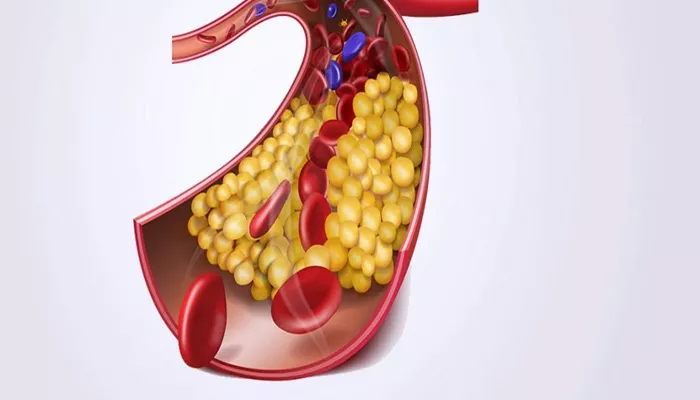
Liver Fat Accumulation: Excess FFAs are taken up by the liver, where they are re-esterified into triglycerides and stored or secreted as very low-density lipoproteins (VLDL). This process increases the levels of circulating triglycerides.
Increased VLDL Production: The liver responds to elevated FFAs by increasing the production and secretion of VLDL particles, which are rich in triglycerides. This contributes to hypertriglyceridemia, a key feature of hyperlipidemia.
SEE ALSO: How Often to Screen for Hyperlipidemia
2. Altered Lipoprotein Metabolism
Lipoproteins are particles that transport lipids through the bloodstream. They include chylomicrons, VLDL, low-density lipoprotein (LDL), and high-density lipoprotein (HDL). Insulin resistance affects the metabolism of these lipoproteins in several ways:
Increased VLDL and LDL: As mentioned, insulin resistance leads to increased production of VLDL by the liver. VLDL particles are eventually converted to LDL particles, which carry cholesterol. Elevated VLDL production thus contributes to increased LDL levels, a characteristic of hyperlipidemia.
Decreased HDL: Insulin resistance is associated with reduced levels of HDL cholesterol, which is responsible for reverse cholesterol transport.
HDL removes excess cholesterol from tissues and transports it to the liver for excretion. Lower HDL levels reduce this protective mechanism, contributing to atherosclerosis risk.
3. Impaired Lipoprotein Lipase Activity
Lipoprotein lipase (LPL) is an enzyme that plays a critical role in the metabolism of triglyceride-rich lipoproteins, such as chylomicrons and VLDL. LPL hydrolyzes triglycerides in these lipoproteins into free fatty acids, which can be taken up by tissues for energy or storage. Insulin normally enhances LPL activity; however, in insulin-resistant states, this regulatory effect is diminished. The resulting impaired LPL activity leads to:
Reduced Triglyceride Clearance: Decreased LPL activity means that triglycerides in VLDL and chylomicrons are not efficiently broken down, leading to elevated levels of circulating triglycerides.
Increased Remnant Particles: Impaired LPL activity also leads to the accumulation of remnant lipoprotein particles, which are partially metabolized VLDL and chylomicrons. These remnants are atherogenic and contribute to cardiovascular disease risk.
4. Hepatic Insulin Resistance and Dyslipidemia
The liver plays a central role in lipid metabolism, and hepatic insulin resistance significantly contributes to hyperlipidemia.
In a healthy state, insulin suppresses gluconeogenesis (the production of glucose from non-carbohydrate sources) and promotes lipid synthesis in the liver. In hepatic insulin resistance, these processes are dysregulated:
Increased Gluconeogenesis: Despite high insulin levels, the liver continues to produce glucose, contributing to hyperglycemia. This paradoxical increase in glucose production exacerbates the insulin resistance state.
Enhanced Lipogenesis: Insulin resistance in the liver leads to increased synthesis of fatty acids and triglycerides, contributing to the accumulation of liver fat and the secretion of triglyceride-rich VLDL particles.
5. Inflammation and Oxidative Stress
Chronic low-grade inflammation and oxidative stress are common features of insulin resistance and play a role in the development of hyperlipidemia:
Adipose Tissue Inflammation: Insulin resistance is often accompanied by an inflammatory response in adipose tissue, characterized by the infiltration of immune cells and the release of pro-inflammatory cytokines. These cytokines interfere with insulin signaling and exacerbate insulin resistance.
Oxidative Stress: Insulin resistance is associated with increased oxidative stress, which can damage lipids, proteins, and DNA. Oxidative stress contributes to the modification of lipoproteins, making them more atherogenic and promoting the development of cardiovascular disease.
6. Genetic and Environmental Factors
Both genetic predisposition and environmental factors, such as diet and physical activity, influence the development of insulin resistance and hyperlipidemia. Genetic factors can affect the expression and function of proteins involved in insulin signaling and lipid metabolism.
Environmental factors, such as a diet high in saturated fats and sugars, sedentary behavior, and obesity, contribute to the development of insulin resistance and dyslipidemia.
Clinical Implications And Management
Understanding the link between insulin resistance and hyperlipidemia has important clinical implications for the prevention and management of metabolic disorders and cardiovascular disease. Key strategies include:
1. Lifestyle Modifications
Diet: Adopting a diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can improve insulin sensitivity and lipid profiles. Reducing the intake of saturated fats, trans fats, and refined sugars is particularly important.
Physical Activity: Regular physical activity enhances insulin sensitivity and promotes lipid metabolism. Both aerobic exercise and resistance training are beneficial.
Weight Management: Achieving and maintaining a healthy weight can improve insulin sensitivity and reduce hyperlipidemia.
2. Pharmacological Interventions
Insulin Sensitizers: Medications such as metformin and thiazolidinediones improve insulin sensitivity and can help manage both insulin resistance and hyperlipidemia.
Lipid-Lowering Agents: Statins, fibrates, and other lipid-lowering medications can be used to reduce elevated lipid levels and lower cardiovascular risk.
Anti-Inflammatory Agents: Therapies targeting inflammation and oxidative stress may also be beneficial in managing insulin resistance and hyperlipidemia.
3. Regular Monitoring and Early Intervention
Regular monitoring of blood glucose and lipid levels is essential for individuals at risk of or diagnosed with insulin resistance and hyperlipidemia. Early intervention can prevent the progression of metabolic disorders and reduce the risk of cardiovascular complications.
Conclusion
Insulin resistance and hyperlipidemia are intricately linked metabolic conditions with significant health implications. The mechanisms underlying this relationship involve complex interactions between glucose and lipid metabolism, impaired enzyme activity, inflammation, and genetic and environmental factors. Understanding these mechanisms provides a foundation for effective prevention and management strategies, emphasizing the importance of lifestyle modifications, pharmacological interventions, and regular monitoring.