Hyperlipidemia, often referred to as high cholesterol, is a medical condition characterized by elevated levels of lipids (fats) in the blood. Lipids include cholesterol and triglycerides, which are essential for various bodily functions but can become harmful when present in excess. This condition is a significant risk factor for cardiovascular diseases, including coronary artery disease, stroke, and peripheral artery disease.
What Body System Is Hyperlipidemia?
1. The Circulatory System and Hyperlipidemia
Cardiovascular Implications
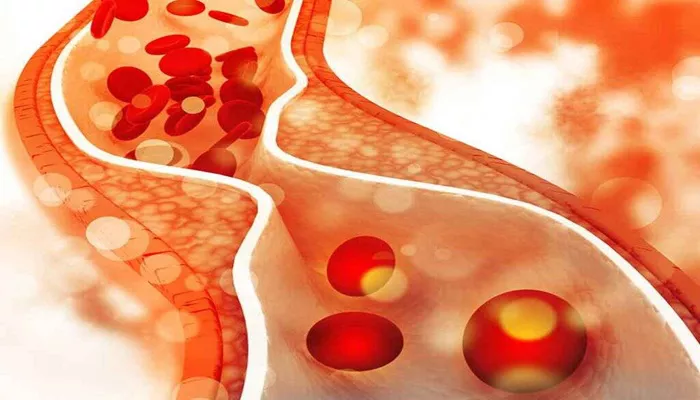
Hyperlipidemia primarily affects the circulatory system, encompassing the heart and blood vessels. The circulatory system’s main function is to transport blood, nutrients, oxygen, and waste products throughout the body. When lipid levels are high, they can lead to the development of atherosclerosis, a condition where plaque builds up inside the arteries. Plaque is composed of fat, cholesterol, calcium, and other substances found in the blood. Over time, this buildup narrows the arteries, restricting blood flow and increasing the risk of heart attack and stroke.
Lipid Metabolism
Lipids are transported in the blood by lipoproteins, which are complexes of lipids and proteins. The main types of lipoproteins include low-density lipoprotein (LDL), high-density lipoprotein (HDL), and very low-density lipoprotein (VLDL). LDL is often referred to as “bad cholesterol” because it can lead to plaque buildup in the arteries, while HDL is known as “good cholesterol” because it helps remove cholesterol from the bloodstream. The balance between these lipoproteins is crucial for maintaining cardiovascular health.
SEE ALSO: Why Does Von Gierke Cause Hyperlipidemia?
2. Endocrine System and Hyperlipidemia
Hormonal Regulation of Lipid Levels
The endocrine system, which includes glands such as the pancreas, thyroid, and adrenal glands, also plays a vital role in lipid metabolism. Hormones produced by these glands regulate various aspects of lipid synthesis, breakdown, and storage.
For instance, insulin, a hormone produced by the pancreas, influences lipid metabolism by promoting the uptake of glucose and its conversion into fatty acids for storage in adipose tissue.
Thyroid Hormones
Thyroid hormones, particularly thyroxine (T4) and triiodothyronine (T3), significantly impact lipid metabolism.
Hypothyroidism, a condition where the thyroid gland produces insufficient thyroid hormones, is associated with elevated levels of LDL cholesterol and triglycerides. Conversely, hyperthyroidism, characterized by excessive thyroid hormone production, can lead to reduced lipid levels. Thus, maintaining thyroid hormone balance is essential for healthy lipid levels and overall metabolic health.
3. Digestive System and Hyperlipidemia
Dietary Influence on Lipid Levels
The digestive system is integral to lipid metabolism, as it is responsible for the digestion and absorption of dietary fats.
When dietary intake of fats and cholesterol is excessive, it can contribute to hyperlipidemia. The small intestine absorbs dietary fats, which are then transported to the liver for processing. The liver plays a central role in lipid metabolism, regulating the synthesis, storage, and distribution of lipids throughout the body.
Bile and Lipid Digestion
Bile, produced by the liver and stored in the gallbladder, is essential for the digestion and absorption of dietary fats. It emulsifies fats, making them more accessible to digestive enzymes. Impaired bile production or secretion can disrupt lipid digestion and absorption, potentially leading to abnormalities in lipid levels.
Genetics And Hyperlipidemia
Inherited Lipid Disorders
Genetic factors also influence lipid levels and the risk of hyperlipidemia. Familial hypercholesterolemia (FH) is a genetic disorder characterized by high levels of LDL cholesterol from birth. Individuals with FH have a higher risk of developing atherosclerosis and cardiovascular diseases at an early age. This condition highlights the importance of genetic factors in lipid metabolism and cardiovascular health.
Genetic Variants
Variations in genes involved in lipid metabolism, such as those encoding for apolipoproteins and lipoprotein receptors, can impact an individual’s lipid levels. Understanding these genetic influences can help identify individuals at higher risk for hyperlipidemia and guide personalized treatment strategies.
Lifestyle Factors And Hyperlipidemia
Diet and Physical Activity
Lifestyle choices significantly affect lipid levels and the risk of hyperlipidemia. A diet high in saturated fats, trans fats, and cholesterol can raise LDL cholesterol levels. Conversely, a diet rich in fruits, vegetables, whole grains, and healthy fats, such as those found in nuts, seeds, and fish, can help lower LDL cholesterol and increase HDL cholesterol.
Regular physical activity is also crucial for maintaining healthy lipid levels. Exercise helps increase HDL cholesterol and decrease LDL cholesterol and triglycerides. It also promotes weight management, which is essential for reducing the risk of hyperlipidemia and associated cardiovascular diseases.
Smoking and Alcohol Consumption
Smoking is a significant risk factor for hyperlipidemia and cardiovascular diseases. It lowers HDL cholesterol levels and damages the endothelium, the inner lining of the arteries, promoting atherosclerosis. Quitting smoking can improve lipid levels and reduce the risk of cardiovascular diseases.
Moderate alcohol consumption can have beneficial effects on lipid levels, particularly by raising HDL cholesterol. However, excessive alcohol intake can lead to elevated triglycerides and other health issues. Therefore, moderation is key.
Management And Treatment of Hyperlipidemia
Lifestyle Modifications
The primary approach to managing hyperlipidemia involves lifestyle modifications. Dietary changes, such as reducing the intake of saturated fats, trans fats, and cholesterol, and increasing the consumption of fiber-rich foods, can significantly improve lipid levels. Regular physical activity, weight management, and smoking cessation are also essential components of hyperlipidemia management.
Medications
In some cases, lifestyle modifications alone may not be sufficient to control lipid levels, and medications may be necessary.
Statins are the most commonly prescribed medications for hyperlipidemia. They work by inhibiting an enzyme involved in cholesterol synthesis in the liver, thereby reducing LDL cholesterol levels. Other medications, such as fibrates, niacin, and bile acid sequestrants, may also be used to manage lipid levels.
Conclusion
Hyperlipidemia is a complex condition that primarily affects the circulatory system but is influenced by various other body systems, including the endocrine and digestive systems. Understanding the interplay between these systems and the factors that contribute to hyperlipidemia is crucial for effective management and prevention of cardiovascular diseases.