Ventricular tachycardia (VT) is a type of arrhythmia, or abnormal heart rhythm, characterized by a rapid heartbeat originating from the ventricles, the heart’s lower chambers. This condition can be life-threatening if not managed appropriately. Understanding the types of VT is crucial for accurate diagnosis and effective treatment. In this comprehensive article, we will explore the various types of ventricular tachycardia, their mechanisms, clinical presentations, diagnostic methods, and treatment options.
Types of Ventricular Tachycardia
1. Monomorphic Ventricular Tachycardia
Monomorphic VT is characterized by a consistent QRS complex morphology, meaning the electrical impulses in the ventricles are uniform in shape and size. This type is often associated with structural heart disease, such as ischemic heart disease or cardiomyopathy.
Etiology: The most common causes include scar tissue from a previous myocardial infarction (heart attack) or other structural abnormalities in the heart.
Clinical Presentation: Patients may experience symptoms ranging from palpitations and dizziness to syncope (fainting) or even sudden cardiac arrest.
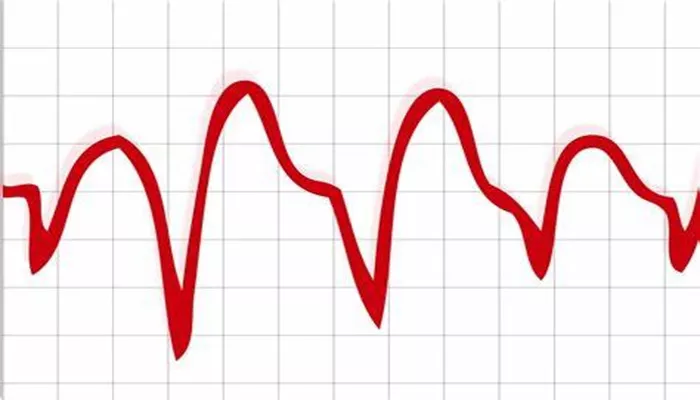
Diagnosis: Diagnosis typically involves electrocardiogram (ECG) analysis, which shows a consistent and uniform QRS complex during VT episodes. Additional tests, such as echocardiography and electrophysiological studies, may be used to assess underlying heart conditions and guide treatment.
Treatment: Treatment options include antiarrhythmic medications, catheter ablation (a procedure that destroys abnormal heart tissue), and implantation of a cardioverter-defibrillator (ICD) for patients at high risk of life-threatening arrhythmias.
2. Polymorphic Ventricular Tachycardia
Polymorphic VT, as the name suggests, features varying QRS complex shapes. This variability in the ECG pattern is indicative of different types of VT and can be caused by several factors.
Etiology: Common causes include congenital long QT syndrome, myocardial ischemia, or electrolyte imbalances. Torsades de Pointes (TdP) is a well-known form of polymorphic VT that often results from prolonged QT interval and is typically associated with a drug-induced effect or genetic predisposition.
Clinical Presentation: Symptoms include palpitations, dizziness, syncope, and, in severe cases, sudden cardiac death.
Diagnosis: The ECG will reveal a changing QRS morphology during the VT episode. Evaluations for underlying causes, such as electrolyte disturbances or medication effects, are crucial for accurate diagnosis.
Treatment: Treatment focuses on correcting the underlying cause. For TdP, discontinuing the offending medication, correcting electrolyte imbalances, and administering intravenous magnesium sulfate are key strategies. In recurrent cases, antiarrhythmic drugs or ICD implantation may be considered.
SEE ALSO: What Is Pheochromocytoma Orthostatic Hypotension?
3. Idiopathic Ventricular Tachycardia
Idiopathic VT refers to cases where the VT occurs without an obvious structural heart disease or identifiable cause. This type is often considered “benign” compared to other forms of VT, but it can still cause significant symptoms.
Etiology: Idiopathic VT is often associated with specific locations in the heart, such as the right ventricular outflow tract (RVOT) or the left ventricular outflow tract (LVOT).
Clinical Presentation: Symptoms may include palpitations, dizziness, or syncope. Despite the absence of structural heart disease, patients can experience distressing symptoms.
Diagnosis: Diagnosis usually involves a thorough evaluation, including ECG, Holter monitoring, and possibly electrophysiological studies to localize the origin of the VT.
Treatment: Treatment options may include antiarrhythmic medications, catheter ablation targeting the specific area of the heart responsible for the arrhythmia, and lifestyle modifications to manage symptoms.
4. Sustained Ventricular Tachycardia
Sustained VT lasts longer than 30 seconds or requires intervention to terminate. It can be either monomorphic or polymorphic and often signifies underlying heart disease.
Etiology: Sustained VT is commonly seen in patients with significant structural heart disease, such as ischemic heart disease or dilated cardiomyopathy.
Clinical Presentation: This form of VT can cause severe symptoms, including chest pain, dizziness, syncope, or sudden cardiac death.
Diagnosis: Diagnosis involves continuous monitoring and documentation of the VT episode. Additional imaging and tests may be required to assess the heart’s structure and function.
Treatment: Immediate treatment may include electrical cardioversion or defibrillation. Long-term management includes antiarrhythmic drugs, catheter ablation, and possibly ICD implantation.
5. Non-Sustained Ventricular Tachycardia
Non-sustained VT lasts less than 30 seconds and may occur sporadically. It is often less symptomatic but can indicate underlying heart issues.
Etiology: Non-sustained VT can occur in patients with structural heart disease, but it may also be seen in individuals with otherwise healthy hearts.
Clinical Presentation: Patients might experience transient symptoms, such as palpitations or dizziness. However, many episodes are asymptomatic.
Diagnosis: Diagnosis is typically made using Holter monitoring or event recorders that capture short bursts of VT.
Treatment: Treatment depends on the frequency and severity of episodes. For symptomatic cases, antiarrhythmic medications or lifestyle changes may be recommended. In asymptomatic cases with low risk, treatment may not be necessary.
Diagnostic Approach to Ventricular Tachycardia
Diagnosing VT involves a combination of patient history, physical examination, and advanced diagnostic tests. Key diagnostic methods include:
Electrocardiogram (ECG): Essential for identifying the type of VT based on the QRS complex morphology and duration.
Holter Monitoring: Provides a continuous ECG recording over 24-48 hours to capture intermittent VT episodes.
Electrophysiological Study: A procedure that maps the electrical activity of the heart to identify and localize abnormal electrical pathways.
Imaging Studies: Echocardiography, MRI, or CT scans may be used to evaluate structural heart abnormalities that could contribute to VT.
Management And Treatment
Effective management of VT requires a tailored approach based on the type and underlying cause of the arrhythmia.
General treatment strategies include:
Medications: Antiarrhythmic drugs are often used to control or prevent VT episodes. The choice of medication depends on the VT type and patient-specific factors.
Catheter Ablation: This procedure targets and destroys the abnormal electrical pathways responsible for VT. It is particularly effective for monomorphic and idiopathic VTs.
Implantable Cardioverter-Defibrillator (ICD): An ICD is used in patients at high risk of sudden cardiac death to automatically detect and correct life-threatening arrhythmias.
Lifestyle Modifications: Addressing risk factors such as hypertension, ischemic heart disease, and electrolyte imbalances can help manage VT.
Conclusion
Ventricular tachycardia is a complex arrhythmia with various types, each requiring specific diagnostic and treatment strategies. Understanding the differences between monomorphic, polymorphic, idiopathic, sustained, and non-sustained VT is crucial for effective management and improving patient outcomes. Through a combination of advanced diagnostics, targeted therapies, and lifestyle modifications, cardiologists can help patients manage VT and reduce the risk of adverse events.