Arrhythmias, or irregular heartbeats, can significantly affect a person’s quality of life and even pose life-threatening risks.
The heart’s rhythm is controlled by electrical signals that prompt the heart to contract and pump blood effectively. When these signals are disrupted, it leads to arrhythmias. A pacemaker is a medical device that can help manage and correct these irregularities. This article will delve into the mechanics of how a pacemaker corrects arrhythmia, its types, implantation procedures, and its impact on patients’ lives.
Types of Arrhythmias
Atrial Fibrillation (AFib): The most common type of serious arrhythmia, characterized by rapid and irregular beating of the atrial chambers.
Bradycardia: Slow heart rate, usually below 60 beats per minute.
Tachycardia: Fast heart rate, typically above 100 beats per minute.
Ventricular Fibrillation: A severe form of arrhythmia that causes chaotic electrical impulses in the ventricles.
Symptoms And Risks
Symptoms of arrhythmias can include palpitations, dizziness, shortness of breath, chest pain, and fatigue. Severe arrhythmias can lead to stroke, heart failure, or sudden cardiac arrest.
The Role of A Pacemaker
What is a Pacemaker?
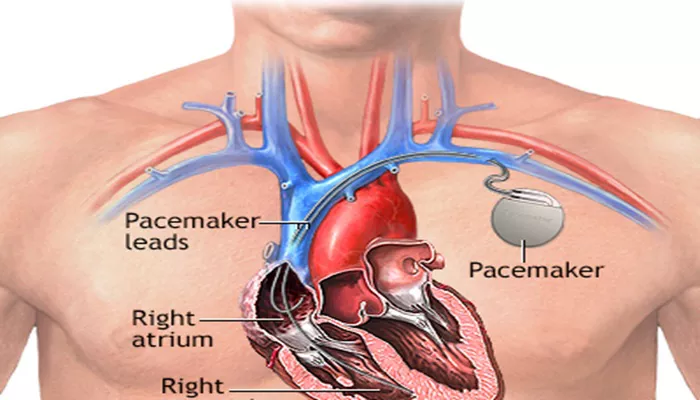
A pacemaker is a small electronic device implanted in the chest or abdomen to help regulate abnormal heart rhythms. It consists of a pulse generator (containing the battery and electronic circuits) and leads (wires that deliver electrical impulses to the heart).
SEE ALSO: How to Identify Sinus Arrhythmia on ECG
Types of Pacemakers
Single-chamber Pacemaker: Uses one lead, typically placed in the right ventricle.
Dual-chamber Pacemaker: Uses two leads, placed in the right atrium and right ventricle, allowing better coordination between the two chambers.
Biventricular Pacemaker: Also known as a cardiac resynchronization therapy (CRT) device, it uses three leads to stimulate both ventricles and the right atrium, used in patients with heart failure.
How A Pacemaker Corrects Arrhythmia
Regulating Heartbeats
A pacemaker corrects arrhythmia by delivering precise electrical impulses to the heart muscle, ensuring a regular and adequate heart rate. Here’s how it works:
Sensing: The pacemaker monitors the heart’s natural electrical activity.
It is programmed to recognize abnormal heart rhythms.
Pacing: When the pacemaker detects an abnormality, it sends electrical impulses through the leads to the heart to prompt a contraction at the correct time.
Rate-responsive Pacing: Modern pacemakers can adjust the pacing rate based on the patient’s activity level, ensuring the heart rate increases during exercise and decreases during rest.
Detailed Mechanism
Bradycardia Correction: In cases of slow heart rate, the pacemaker ensures the heart beats at a minimum rate by sending impulses when the natural heart rate falls below a set threshold.
Tachycardia and AFib: For fast or irregular rhythms, pacemakers can deliver timed electrical stimuli to restore normal rhythm or prevent the heart from beating too rapidly.
Implantation Procedure
Pre-Procedure Preparation
Before the procedure, patients undergo several evaluations, including blood tests, electrocardiograms (ECGs), and imaging studies to determine the precise requirements for the pacemaker.
The Procedure
Anesthesia: The patient is usually given local anesthesia to numb the implantation area, and sometimes mild sedation.
Incision and Lead Placement: A small incision is made near the collarbone, and leads are guided through a vein to the heart under fluoroscopy.
Connection and Testing: The leads are connected to the pulse generator, which is then tested to ensure proper function.
Generator Placement: The pulse generator is placed under the skin, and the incision is closed.
Post-Procedure Care
Patients are monitored for a few hours to a day post-implantation. Instructions are given on how to care for the incision site, activity restrictions, and follow-up appointments.
Living with A Pacemaker
Recovery and Adjustment
Most patients return to normal activities within a few weeks. They are advised to avoid strenuous activities and heavy lifting for some time to allow the leads to settle securely.
Regular Monitoring
Pacemakers require regular check-ups to ensure they function correctly and to monitor battery life. Modern devices can be checked remotely.
Lifestyle Considerations
Patients with pacemakers should be aware of potential electromagnetic interference from certain devices and environments.
They are advised to keep cell phones and MP3 players at least six inches away from the pacemaker and to avoid strong magnetic fields.
Benefits and Impact
Pacemakers significantly improve the quality of life for patients with arrhythmias, reducing symptoms and preventing complications like stroke and heart failure. They enable patients to lead more active and normal lives.
Advances in Pacemaker Technology
Leadless Pacemakers
Recent advancements have introduced leadless pacemakers, which are smaller and are implanted directly into the heart without leads.
These devices reduce the risk of lead-related complications and are less invasive to implant.
MRI-compatible Pacemakers
Newer pacemakers are designed to be compatible with MRI scans, allowing patients to undergo this imaging procedure safely, which is crucial for diagnosing various conditions.
Remote Monitoring
Modern pacemakers are equipped with wireless technology that allows for remote monitoring, providing continuous data to healthcare providers and enabling timely interventions if abnormalities are detected.
Conclusion
Pacemakers play a crucial role in correcting arrhythmias by ensuring a regular and adequate heart rate, significantly improving patients’ quality of life and reducing the risk of serious complications. With ongoing advancements in technology, pacemakers continue to become more effective, safer, and more convenient for patients, marking significant strides in the management of heart rhythm disorders.