Orthostatic hypotension (OH) is a common non-motor symptom in Parkinson’s disease (PD) that can significantly impact the quality of life for patients. It is characterized by a sudden drop in blood pressure when a person stands up from a sitting or lying position, leading to dizziness, lightheadedness, and even fainting. Managing OH in PD patients requires a multifaceted approach. Here are five effective treatments for orthostatic hypotension in Parkinson’s disease.
1. Pharmacological Treatments
Medications to Increase Blood Pressure
Several medications can help manage OH by increasing blood pressure. These include:
Fludrocortisone: A synthetic corticosteroid that increases blood volume and blood pressure by promoting sodium retention and expanding plasma volume. It is often one of the first-line treatments for OH in PD.
Midodrine: An alpha-adrenergic agonist that constricts blood vessels, thereby increasing blood pressure. It is particularly effective in treating OH and is commonly prescribed for PD patients.
Droxidopa: A norepinephrine precursor that increases norepinephrine levels, which helps improve blood vessel tone and raise blood pressure. Droxidopa has shown significant efficacy in managing OH in PD.
These medications need to be carefully dosed and monitored by healthcare professionals to avoid adverse effects like supine hypertension (high blood pressure while lying down).
SEE ALSO: Why Does Exercise Help Lower Blood Pressure?
Medications to Reduce PD Symptoms
Adjusting PD medications can also help manage OH. Some PD medications, such as levodopa and dopamine agonists, can exacerbate OH. Modifying the dosage or timing of these medications, or switching to alternatives with a lower risk of causing OH, can help alleviate symptoms. For example, reducing the dose of levodopa or switching to extended-release formulations may help.
2. Non-Pharmacological Interventions
Dietary Adjustments
Dietary modifications can significantly impact blood pressure regulation. Key strategies include:
Increased Salt Intake: Consuming more salt can help raise blood pressure by increasing blood volume. However, this should be done under medical supervision to avoid potential complications like heart failure or kidney disease.
Increased Fluid Intake: Drinking more fluids can help maintain blood volume and prevent dehydration, which can exacerbate OH. Patients are often advised to drink at least 2-3 liters of water daily.
Frequent Small Meals: Large meals can divert blood flow to the digestive system, leading to postprandial hypotension.
Eating smaller, more frequent meals can help prevent significant drops in blood pressure after eating.
Compression Garments
Wearing compression stockings or abdominal binders can help prevent blood from pooling in the lower extremities, thus improving blood flow and increasing blood pressure. These garments apply external pressure, which can be particularly effective when standing or during prolonged periods of sitting.
3. Physical Countermaneuvers
Exercise and Physical Activity
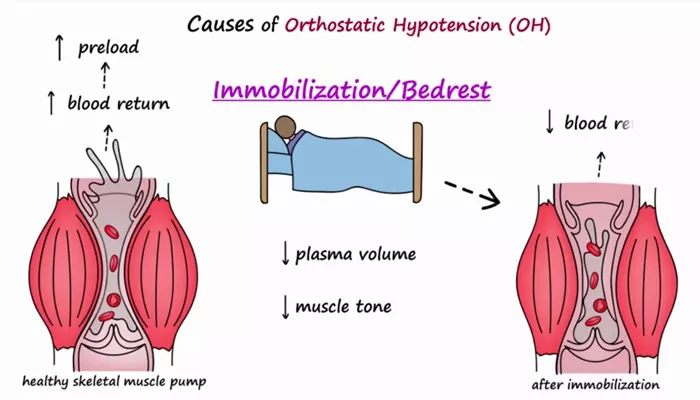
Regular physical activity can help improve cardiovascular fitness and blood pressure regulation. Specific exercises that target muscle strength and endurance can be particularly beneficial. For instance, lower body exercises like leg presses and squats can help enhance blood return to the heart.
Physical Countermaneuvers
Patients can be taught specific physical maneuvers to counteract the symptoms of OH. These include:
Leg Crossing and Squatting: Crossing the legs while standing or performing squats can increase blood return to the heart and prevent a sudden drop in blood pressure.
Isometric Handgrip Exercises: Squeezing a handgrip or a tennis ball can increase blood pressure temporarily and help alleviate symptoms of OH.
Gradual Position Changes: Moving slowly from lying to sitting and from sitting to standing can give the body time to adjust and reduce the risk of sudden blood pressure drops.
4. Lifestyle Modifications
Posture and Positioning
Adopting specific postural strategies can help manage OH symptoms:
Head-Up Tilt: Sleeping with the head of the bed elevated can help reduce the severity of OH by preventing fluid accumulation in the lower body during the night.
Avoiding Prolonged Standing: Reducing the time spent standing still and taking breaks to sit or lie down can help manage symptoms.
Avoiding Hot Environments: Heat can exacerbate OH by causing vasodilation (widening of blood vessels). Avoiding hot baths, showers, and environments can help prevent drops in blood pressure.
Monitoring and Education
Educating patients and caregivers about OH and its triggers is crucial for effective management. Patients should be aware of the signs and symptoms of OH and know when to seek medical attention. Regular blood pressure monitoring at home can help track the effectiveness of treatments and make necessary adjustments.
5. Advanced Therapeutic Options
Volume Expansion Therapies
In severe cases of OH that do not respond to standard treatments, more advanced therapies may be considered. These include:
Intravenous Fluids: Administering intravenous fluids can help rapidly increase blood volume and blood pressure in acute settings.
Erythropoietin: This hormone, which stimulates red blood cell production, can help increase blood volume and improve symptoms in some patients with OH.
Neurostimulation
Emerging therapies like neurostimulation have shown promise in managing OH. Techniques such as baroreflex activation therapy, which involves stimulating the baroreceptors (pressure sensors in the blood vessels), can help regulate blood pressure. Although still under investigation, these therapies offer potential for future treatment options.
Customized Treatment Plans
Given the complexity of OH in PD, treatment plans should be highly individualized. Collaborating with a multidisciplinary team, including neurologists, cardiologists, and physical therapists, can help create a comprehensive and effective management strategy tailored to each patient’s needs.
Conclusion
Managing orthostatic hypotension in Parkinson’s disease requires a multifaceted approach that combines pharmacological treatments, non-pharmacological interventions, physical countermeasures, lifestyle modifications, and advanced therapies.
Each patient’s treatment plan should be individualized, considering their specific symptoms and overall health status. With the right combination of treatments, patients with PD can achieve better control over their blood pressure and improve their quality of life. Regular follow-up and monitoring are essential to ensure the effectiveness of the treatment plan and make necessary adjustments.