Heart function is crucial to overall health and well-being, as it affects the body’s ability to supply oxygen and nutrients to vital organs and tissues. When heart function is compromised, as evidenced by a reduced ejection fraction (EF), it can have significant implications for a person’s lifespan and quality of life. This article explores the prognosis for individuals with 45% heart function, providing insights into the potential outcomes, factors influencing longevity, and management strategies.
What Is Heart Function?
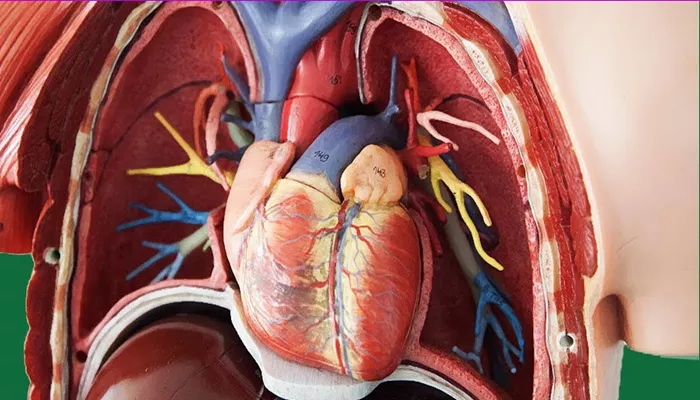
Heart function, often assessed through ejection fraction (EF), measures how well the heart pumps blood. EF is expressed as a percentage, representing the proportion of blood ejected from the left ventricle with each heartbeat. A normal EF ranges from 55% to 70%.
An EF of 45% indicates reduced heart function, often associated with heart failure or other cardiovascular conditions. The severity of this reduction can influence the prognosis and life expectancy of affected individuals.
see also: What Does A Coronary Artery Spasm Feel Like?
Factors Influencing Longevity with 45% Heart Function
Several factors impact how long a person can live with 45% heart function. These include:
Underlying Cause: The cause of reduced heart function plays a critical role in determining prognosis. Conditions such as coronary artery disease, hypertension, cardiomyopathy, and valvular heart disease can lead to decreased EF. The specific etiology can influence treatment options and overall outcomes.
Symptoms and Functional Capacity: Individuals with reduced heart function may experience symptoms such as shortness of breath, fatigue, and swelling. The presence and severity of these symptoms, along with the individual’s functional capacity, can affect life expectancy. Those who can maintain an active lifestyle may have a better prognosis than those with severe limitations.
Response to Treatment: Treatment strategies, including medication, lifestyle changes, and surgical interventions, can significantly impact outcomes. Effective management can improve symptoms, enhance quality of life, and potentially extend lifespan.
Comorbidities: The presence of other medical conditions, such as diabetes, renal dysfunction, or chronic obstructive pulmonary disease (COPD), can complicate management and affect prognosis. Managing comorbidities is essential for optimizing outcomes.
Age and Overall Health: Age and general health status play a role in how well individuals cope with reduced heart function. Younger individuals with fewer comorbidities may have a better outlook compared to older adults with multiple health issues.
Prognosis for Individuals with 45% Heart Function
Prognosis varies widely among individuals with reduced heart function. Studies suggest that individuals with an EF of 45% can have a variable life expectancy depending on the factors mentioned above.
Survival Rates: Research indicates that individuals with heart failure and an EF around 45% have a range of survival rates.
For instance, the annual mortality rate for individuals with heart failure can range from 5% to 20%, depending on the severity of symptoms and other health conditions. Long-term survival rates are influenced by effective treatment and lifestyle management.
Quality of Life: Even with reduced EF, many individuals can maintain a good quality of life with appropriate treatment and lifestyle adjustments. Advances in medical therapies and interventions have improved outcomes for those with heart failure.
Management Strategies
Effective management is crucial for improving prognosis and quality of life in individuals with reduced heart function. Key strategies include:
Medications: Medications such as ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists are commonly used to manage heart failure and improve heart function. These drugs help reduce symptoms, prevent disease progression, and enhance overall heart performance.
Lifestyle Changes: Adopting a heart-healthy lifestyle is essential. This includes a balanced diet, regular physical activity, weight management, and avoiding smoking and excessive alcohol consumption. Lifestyle changes can help reduce the strain on the heart and improve overall health.
Monitoring and Follow-Up: Regular monitoring and follow-up with a cardiologist are vital for managing heart function.
This includes routine check-ups, echocardiograms, and other diagnostic tests to assess heart performance and adjust treatment as needed.
Advanced Therapies: In some cases, advanced therapies such as implantable devices (e.g., pacemakers, defibrillators) or surgical interventions (e.g., heart valve repair, coronary artery bypass grafting) may be necessary to improve heart function and enhance survival.
Patient Education: Educating patients about their condition, treatment options, and self-care strategies is crucial for effective management.
Empowering individuals with knowledge helps them make informed decisions and actively participate in their care.
Conclusion
Living with 45% heart function presents challenges, but with appropriate management and treatment, individuals can lead fulfilling lives and potentially extend their lifespan. The prognosis depends on various factors, including the underlying cause, symptom severity, response to treatment, and overall health. By working closely with healthcare providers, adhering to treatment plans, and making lifestyle adjustments, individuals with reduced heart function can achieve better outcomes and improve their quality of life.