Myocarditis, an inflammation of the heart muscle, can be caused by a variety of factors, including infections, autoimmune conditions, and exposure to certain toxins. Among these, bacterial infections are significant contributors to myocarditis.
Understanding which bacteria are most commonly associated with this condition can aid in prevention, diagnosis, and treatment. This article delves into the various bacterial agents responsible for myocarditis, their mechanisms of causing the disease, and the clinical implications of these infections.
Understanding Myocarditis
Myocarditis involves inflammation of the myocardium, the muscular middle layer of the heart wall. The condition can affect heart function, leading to symptoms such as chest pain, fatigue, shortness of breath, and in severe cases, heart failure.
Diagnosis often involves a combination of clinical presentation, imaging studies, and sometimes endomyocardial biopsy.
Bacterial Causes of Myocarditis
Streptococcus Species
Streptococcus pyogenes: This bacterium, commonly known for causing strep throat, can also lead to myocarditis. The pathogenesis often involves post-streptococcal sequelae, such as rheumatic fever. Rheumatic fever can result in acute myocarditis and chronic rheumatic heart disease, where the heart valves are damaged, leading to long-term cardiac issues.
Streptococcus pneumoniae: Known primarily for causing pneumonia, Streptococcus pneumoniae has also been implicated in myocarditis. While less common, it can cause significant disease, especially in individuals with weakened immune systems or underlying health conditions.
SEE ALSO: What Is Sarcoid Myocarditis?
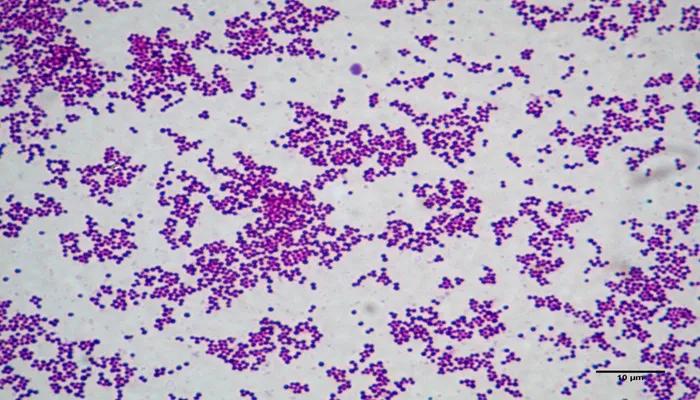
Staphylococcus Species
Staphylococcus aureus: This pathogen is a well-known cause of skin and soft tissue infections but can also lead to myocarditis, particularly in cases where it spreads from a systemic infection. Staphylococcus aureus can cause severe myocarditis through hematogenous dissemination or as a complication of infective endocarditis.
Staphylococcus epidermidis: Although typically considered a less virulent coagulase-negative staphylococcus, Staphylococcus epidermidis can cause myocarditis in the context of prosthetic devices or indwelling catheters, where it acts as an opportunistic pathogen.
Corynebacterium diphtheriae
Corynebacterium diphtheriae: The bacterium responsible for diphtheria can also lead to myocarditis, particularly in severe cases of the disease. Diphtheritic myocarditis is a consequence of the toxin produced by the bacterium, which affects the heart muscle.
Borrelia Burgdorferi
Borrelia burgdorferi: This spirochete is the causative agent of Lyme disease. Myocarditis can occur in the context of Lyme disease, particularly in its later stages. Lyme carditis is a specific manifestation where the bacterium invades the heart tissue, causing varying degrees of myocarditis and heart block.
Mycobacterium Tuberculosis
Mycobacterium tuberculosis: Tuberculous myocarditis is rare but can occur in patients with disseminated tuberculosis.
The infection can lead to granulomatous inflammation of the heart tissue, presenting as myocarditis.
Mechanisms of Bacterial-Induced Myocarditis
Bacteria can cause myocarditis through several mechanisms:
Direct Infection: Bacteria can directly invade and damage heart muscle cells, leading to inflammation. This is often seen with Staphylococcus aureus and Corynebacterium diphtheriae.
Toxin-Mediated Injury: Some bacteria produce toxins that can damage the heart muscle. For instance, the diphtheria toxin affects cardiac cells, leading to myocarditis.
Immune-Mediated Injury: In some cases, the immune response to a bacterial infection can lead to myocarditis. For example, the immune response to Streptococcus pyogenes in rheumatic fever can result in inflammation of the myocardium.
Clinical Implications And Management
Understanding the bacterial etiology of myocarditis is crucial for effective management. Treatment typically involves:
Antibiotic Therapy: Targeted antibiotic treatment is essential for bacterial infections. The choice of antibiotic depends on the specific pathogen and its susceptibility.
Supportive Care: Patients with myocarditis may require supportive care, including medications to manage heart failure symptoms and other complications.
Monitoring and Follow-Up: Regular follow-up is necessary to monitor cardiac function and adjust treatment as needed.
Conclusion
Bacterial myocarditis, while less common than viral myocarditis, represents a significant clinical challenge. Streptococcus species, Staphylococcus aureus, Corynebacterium diphtheriae, Borrelia burgdorferi, and Mycobacterium tuberculosis are among the notable bacterial agents associated with myocarditis. Understanding these pathogens and their mechanisms of causing myocarditis helps in early diagnosis and effective management of the condition. Continued research and vigilance are essential for improving outcomes in patients affected by bacterial myocarditis.