Hypertension, or high blood pressure, is a prevalent condition that affects millions of people worldwide. It’s often referred to as a “silent killer” because it typically does not present symptoms until significant damage has occurred. One of the most severe consequences of uncontrolled hypertension is myocardial infarction (MI), commonly known as a heart attack. This article explores the relationship between hypertension and myocardial infarction, delving into the mechanisms by which high blood pressure contributes to heart attacks, risk factors, and prevention strategies.
1. The Basics of Hypertension And Myocardial Infarction
What is Hypertension?
Hypertension is characterized by consistently elevated blood pressure levels. Blood pressure is measured in millimeters of mercury (mmHg) and recorded as two numbers: systolic pressure (the force of blood against the artery walls when the heart beats) and diastolic pressure (the force of blood against the artery walls when the heart rests between beats). A normal blood pressure reading is typically around 120/80 mmHg. Hypertension is diagnosed when blood pressure readings are consistently 140/90 mmHg or higher.
SEE ALSO: How to Lower Your Blood Pressure Without Medicine
What is Myocardial Infarction?
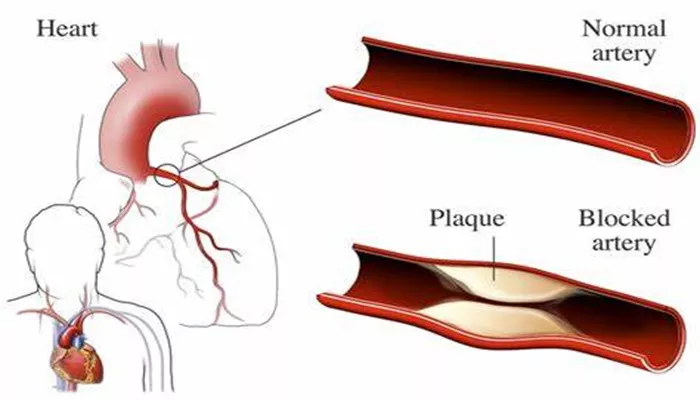
Myocardial infarction (MI) occurs when blood flow to a part of the heart muscle is obstructed for a prolonged period, leading to tissue damage or death. The obstruction is usually caused by a blood clot that forms in a coronary artery that has been narrowed or blocked by atherosclerosis—a condition where fatty deposits, known as plaques, build up on the artery walls.
2. The Pathophysiology of Hypertension And Myocardial Infarction
How Hypertension Contributes to Atherosclerosis
Chronic hypertension can lead to the development of atherosclerosis. High blood pressure damages the inner lining of the arteries (endothelium), making them more susceptible to plaque formation. When the endothelium is damaged, it becomes easier for cholesterol, fats, and other substances to accumulate and form plaques. These plaques can narrow and harden the arteries, reducing blood flow and increasing the risk of blood clots.
Increased Workload on the Heart
Hypertension forces the heart to work harder to pump blood through the narrowed arteries. Over time, this increased workload can lead to left ventricular hypertrophy (LVH), a condition where the heart’s left ventricle thickens and becomes less efficient. LVH increases the heart’s oxygen demand while simultaneously decreasing its ability to deliver oxygen-rich blood to the heart muscle. This imbalance can contribute to ischemia (reduced blood flow) and increase the risk of myocardial infarction.
Endothelial Dysfunction and Hypercoagulability
Hypertension can also cause endothelial dysfunction, characterized by a reduced ability of the endothelium to regulate blood vessel tone and maintain blood flow. Endothelial dysfunction is associated with an increased risk of clot formation.
Moreover, high blood pressure can increase blood viscosity (thickness) and promote a hypercoagulable state, further elevating the risk of thrombosis (blood clots) in the coronary arteries.
3. Risk Factors And Complications
Modifiable Risk Factors
Several factors can exacerbate the impact of hypertension on heart health, including:
High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can accelerate plaque formation in the arteries.
Smoking: Tobacco use damages blood vessels and promotes the formation of arterial plaques.
Diabetes: High blood sugar levels can damage blood vessels and contribute to the development of atherosclerosis.
Obesity: Excess body weight increases the risk of hypertension, diabetes, and other cardiovascular diseases.
Physical Inactivity: A sedentary lifestyle contributes to weight gain and poor cardiovascular health.
Non-Modifiable Risk Factors
Certain factors cannot be changed but can still influence the risk of myocardial infarction:
Age: The risk of cardiovascular disease increases with age.
Genetics: A family history of heart disease or hypertension can predispose individuals to these conditions.
Gender: Men are generally at higher risk for heart attacks at a younger age, but the risk for women increases and may surpass that of men after menopause.
4. Prevention And Management
Controlling Blood Pressure
Effective management of hypertension is crucial in reducing the risk of myocardial infarction. Strategies include:
Lifestyle Modifications: Adopting a heart-healthy diet (low in sodium and rich in fruits, vegetables, and whole grains), engaging in regular physical activity, limiting alcohol intake, and quitting smoking.
Medication: Various antihypertensive medications, such as ACE inhibitors, beta-blockers, calcium channel blockers, and diuretics, may be prescribed to manage blood pressure.
Monitoring and Early Intervention
Regular monitoring of blood pressure is essential for detecting and managing hypertension early. Individuals with elevated blood pressure should undergo routine cardiovascular screenings to assess their risk for myocardial infarction and other heart-related issues.
Managing Coexisting Conditions
Addressing other risk factors, such as high cholesterol and diabetes, is vital in reducing the overall risk of myocardial infarction. Lifestyle changes, medications, and regular check-ups can help manage these conditions effectively.
5. Conclusion
Hypertension is a significant risk factor for myocardial infarction, and understanding the mechanisms by which high blood pressure contributes to heart attacks is crucial for prevention and management. By addressing modifiable risk factors, managing hypertension effectively, and working closely with healthcare providers, individuals can reduce their risk of myocardial infarction and improve their overall cardiovascular health. Early intervention and a commitment to a heart-healthy lifestyle are key components in preventing the devastating effects of hypertension on the heart.