Acute myocarditis is an inflammatory condition affecting the heart muscle (myocardium), typically triggered by viral infections, autoimmune diseases, or other factors. It presents a complex clinical picture and requires prompt, targeted management to improve outcomes and prevent complications. This article explores the latest approaches to treating acute myocarditis, from initial diagnosis to advanced therapeutic strategies.
Recognizing Acute Myocarditis
Acute myocarditis often begins with flu-like symptoms such as fever, fatigue, and malaise. These can be followed by more specific signs such as chest pain, dyspnea (shortness of breath), and arrhythmias (irregular heartbeats). The condition can be misdiagnosed or mistaken for other cardiac disorders, making accurate and timely diagnosis crucial.
SEE ALSO: What Is Sarcoid Myocarditis?
Diagnosis And Initial Evaluation
Clinical Assessment: The first step in diagnosing acute myocarditis is a thorough clinical assessment. Physicians will evaluate symptoms, medical history, and physical examination findings. A detailed history of recent viral infections or autoimmune diseases can provide critical clues.
Laboratory Tests: Blood tests are essential for diagnosing myocarditis. Elevated cardiac biomarkers such as troponin I or T, and brain natriuretic peptide (BNP), indicate myocardial injury. Inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can help assess the level of inflammation.
Electrocardiogram (ECG): An ECG is used to detect electrical abnormalities in the heart. In acute myocarditis, the ECG may show ST-segment elevation, T-wave inversions, or other changes indicative of myocardial inflammation.
Echocardiography: This imaging technique assesses heart function and structure. It can reveal reduced ejection fraction, ventricular dilation, and other features suggestive of myocarditis.
Cardiac MRI: Cardiac magnetic resonance imaging (MRI) is a non-invasive method that provides detailed images of the heart muscle. It is particularly useful for identifying inflammation and myocardial edema.
Endomyocardial Biopsy: In cases where the diagnosis is uncertain, an endomyocardial biopsy may be performed. This procedure involves taking a small sample of heart tissue for histopathological examination, which can confirm the presence of myocarditis.
Treatment Approaches
The treatment of acute myocarditis is multifaceted, aiming to address the underlying cause, manage symptoms, and prevent complications.
Here are the primary strategies:
Supportive Care
Rest: Adequate rest is crucial to reduce the workload on the heart and support recovery.
Monitoring: Continuous monitoring in a hospital setting may be necessary for severe cases to manage arrhythmias and heart failure.
Pharmacological Management
Anti-inflammatory Drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and manage symptoms. However, their use is debated, especially in cases with suspected viral etiology, as they might exacerbate the condition.
Antiviral Medications: If a viral infection is identified as the cause, antiviral therapy might be considered. However, the effectiveness of antiviral drugs in treating myocarditis is still under investigation.
Heart Failure Management: Medications such as ACE inhibitors, beta-blockers, and diuretics are used to manage heart failure symptoms.
These drugs help to reduce the strain on the heart and improve function.
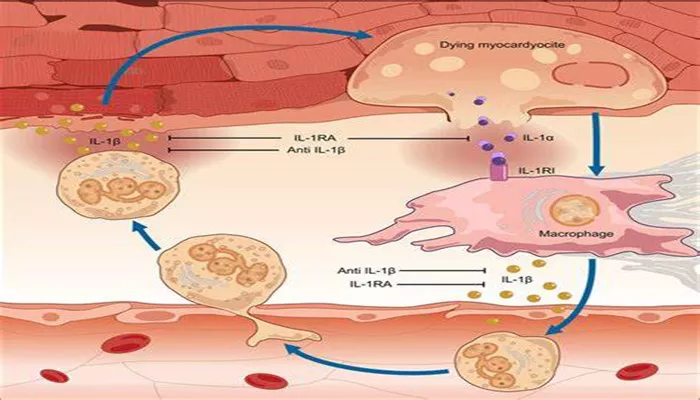
Immunosuppressive Therapy: In cases where autoimmune diseases are suspected, immunosuppressive drugs like azathioprine or cyclosporine may be used to reduce immune-mediated damage.
Advanced Therapies
Intravenous Immunoglobulin (IVIG): IVIG can be administered to modulate the immune response and reduce inflammation in severe cases of myocarditis.
Plasma Exchange: This procedure, also known as plasmapheresis, removes harmful antibodies from the blood and may be beneficial in autoimmune myocarditis.
Mechanical Circulatory Support: In cases of severe heart failure or cardiogenic shock, devices like intra-aortic balloon pumps (IABP) or ventricular assist devices (VADs) may be used to support heart function.
Long-Term Management and Follow-Up
Regular Monitoring: Patients with acute myocarditis require ongoing follow-up to monitor heart function and detect any late-onset complications. Regular echocardiograms and cardiac MRIs may be performed.
Lifestyle Modifications: Patients are advised to make lifestyle changes such as adopting a heart-healthy diet, avoiding excessive physical exertion, and managing stress.
Psychological Support: Chronic illness and recovery from severe conditions like myocarditis can be challenging.
Psychological support and counseling may be beneficial for patients and their families.
Prognosis And Recovery
The prognosis of acute myocarditis varies depending on the severity of the condition, the underlying cause, and the response to treatment. Many patients recover fully with appropriate management, while others may experience persistent cardiac dysfunction or complications. Early diagnosis and treatment are critical for improving outcomes and minimizing long-term effects.
Conclusion
Treating acute myocarditis involves a comprehensive approach that includes diagnosing the condition accurately, managing symptoms, and addressing underlying causes. Advances in medical therapies and technologies have improved the ability to manage this complex condition effectively. By following a tailored treatment plan and ensuring ongoing follow-up, healthcare providers can optimize outcomes and support patients on their path to recovery.