Hyperkalemia, a condition characterized by elevated levels of potassium in the blood, can have significant effects on the cardiovascular system. One of the most concerning complications of hyperkalemia is its potential to cause arrhythmias, which are abnormal heart rhythms that can range from benign to life-threatening. This article delves into the types of arrhythmias associated with hyperkalemia, the underlying mechanisms, and the clinical implications of this condition.
What Is Hyperkalemia?
Hyperkalemia is defined as a serum potassium level greater than 5.0 milliequivalents per liter (mEq/L). Potassium is a critical electrolyte in the body, essential for various physiological processes including the regulation of heartbeat, muscle contractions, and nerve function. Normal potassium levels typically range from 3.5 to 5.0 mEq/L. Levels above this range can disrupt normal cellular functions, particularly in the heart.
Causes of Hyperkalemia
Hyperkalemia can result from several conditions and factors, including:
Renal Impairment: The kidneys play a crucial role in maintaining potassium balance. Renal failure or chronic kidney disease can impair potassium excretion, leading to hyperkalemia.
Medications: Certain medications, such as potassium-sparing diuretics, ACE inhibitors, and angiotensin II receptor blockers (ARBs), can increase potassium levels.
Dietary Intake: Excessive intake of potassium-rich foods or supplements can contribute to hyperkalemia, particularly in individuals with impaired renal function.
Cellular Release: Conditions that cause rapid cell breakdown, such as trauma, burns, or hemolysis, can release large amounts of potassium into the bloodstream.
Hormonal Disorders: Addison’s disease and other disorders affecting aldosterone production can impair potassium excretion.
SEE ALSO: Which Arrhythmia Increases The Risk of Stroke?
The Mechanism of Arrhythmias in Hyperkalemia
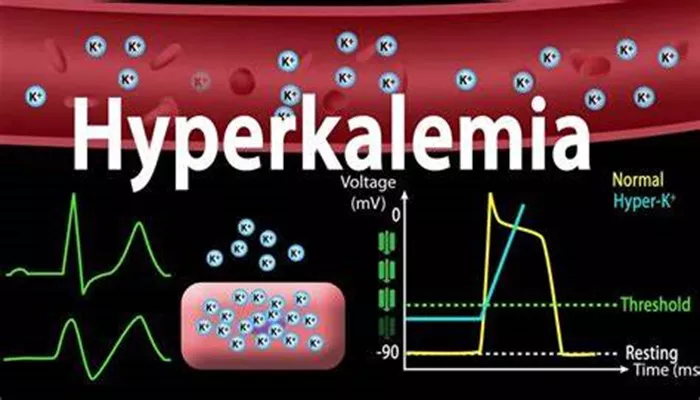
Potassium plays a vital role in the electrical activity of the heart. It is involved in the maintenance of the resting membrane potential and the propagation of action potentials in cardiac cells. Elevated potassium levels can alter these electrical properties, leading to changes in cardiac excitability and conduction.
Effects on Resting Membrane Potential
Hyperkalemia reduces the resting membrane potential of cardiac cells, making them less negative. This depolarization can inactivate sodium channels, which are essential for the initiation and propagation of action potentials. As a result, the conduction velocity of electrical impulses in the heart can slow down, leading to various types of arrhythmias.
Effects on Action Potentials
High potassium levels can shorten the action potential duration by accelerating the repolarization phase. This can lead to changes in the refractory period, the time during which cardiac cells are unable to initiate another action potential.
Alterations in the refractory period can predispose the heart to reentrant arrhythmias, where the electrical impulse continuously circles within the heart tissue, causing sustained abnormal rhythms.
Types of Arrhythmias Caused by Hyperkalemia
Hyperkalemia can cause a range of arrhythmias, from relatively benign to potentially fatal. The severity and type of arrhythmia depend on the degree of potassium elevation and the presence of other underlying cardiac conditions.
1. Sinus Bradycardia
Sinus bradycardia, a slow heart rate originating from the sinoatrial (SA) node, is one of the early manifestations of hyperkalemia. As potassium levels rise, the resting membrane potential of the SA node cells becomes less negative, reducing the rate of spontaneous depolarization. This results in a slower heart rate.
2. Atrioventricular (AV) Block
Hyperkalemia can cause various degrees of AV block, where the conduction of electrical impulses from the atria to the ventricles is impaired. This occurs because elevated potassium levels slow down the conduction through the AV node and the His-Purkinje system. AV blocks can range from first-degree block, with prolonged PR interval, to complete heart block, where no atrial impulses are conducted to the ventricles.
3. Ventricular Tachycardia
Ventricular tachycardia (VT) is a rapid heart rhythm originating from the ventricles. In the context of hyperkalemia, VT can occur due to enhanced automaticity of ventricular cells or reentrant circuits. The shortening of the action potential duration and changes in refractory periods contribute to the development of VT in hyperkalemia.
4. Ventricular Fibrillation
Ventricular fibrillation (VF) is a life-threatening arrhythmia characterized by chaotic and ineffective ventricular contractions. It can result from severe hyperkalemia, where the electrical activity in the ventricles becomes highly disorganized. VF leads to a complete loss of effective cardiac output and requires immediate medical intervention.
5. Asystole
Asystole, or “flatline,” is the absence of any electrical activity in the heart. In extreme cases of hyperkalemia, the depolarization of cardiac cells can be so profound that the heart’s electrical system shuts down completely, resulting in asystole. This condition is rapidly fatal if not promptly treated.
Clinical Implications And Management
The recognition and management of hyperkalemia are critical to preventing arrhythmias and their associated complications. Clinicians must maintain a high index of suspicion for hyperkalemia in patients with risk factors such as renal impairment, medication use, or conditions causing rapid cell turnover.
Diagnosis
Hyperkalemia is diagnosed through serum potassium measurements. Electrocardiogram (ECG) findings can also provide clues to the presence and severity of hyperkalemia. Common ECG changes associated with hyperkalemia include:
Peaked T Waves: Early sign of hyperkalemia due to rapid repolarization.
Prolonged PR Interval: Indicative of slowed AV conduction.
Widened QRS Complex: Reflects delayed ventricular depolarization.
Flattened P Waves: Resulting from slowed atrial depolarization.
Sine Wave Pattern: Severe hyperkalemia, where QRS complexes and T waves merge, indicating impending ventricular fibrillation or asystole.
Treatment
The treatment of hyperkalemia aims to stabilize cardiac membranes, shift potassium into cells, and remove excess potassium from the body. Key interventions include:
Calcium Gluconate: Administered intravenously to stabilize cardiac membranes and reduce the risk of arrhythmias.
Insulin and Glucose: Insulin promotes the uptake of potassium into cells, and glucose is given to prevent hypoglycemia.
Beta-2 Agonists: Medications like albuterol can stimulate potassium uptake into cells.
Sodium Bicarbonate: Used in cases of metabolic acidosis to shift potassium into cells.
Potassium Binders: Medications such as sodium polystyrene sulfonate can bind potassium in the gut and facilitate its excretion.
Dialysis: In severe cases or when other treatments are ineffective, dialysis may be required to remove excess potassium.
Conclusion
Hyperkalemia is a potentially life-threatening condition that can cause a variety of arrhythmias, ranging from sinus bradycardia and AV block to ventricular tachycardia, ventricular fibrillation, and asystole. Understanding the mechanisms by which hyperkalemia affects cardiac electrophysiology is crucial for the timely recognition and management of this condition. Clinicians must be vigilant in monitoring and treating hyperkalemia to prevent arrhythmias and their associated complications. Effective management strategies include stabilizing cardiac membranes, shifting potassium into cells, and removing excess potassium from the body.