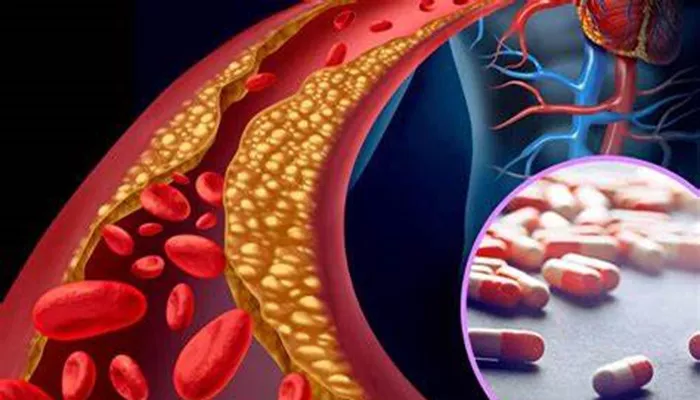
Hyperlipidemia is a medical condition characterized by elevated levels of lipids (fats) in the blood, primarily cholesterol and triglycerides. While primary hyperlipidemia is often due to genetic factors, secondary hyperlipidemia arises from other underlying conditions, lifestyle choices, or medications. Understanding these secondary causes is crucial for effective management and treatment. This article delves into the various secondary causes of hyperlipidemia, exploring how different factors contribute to this condition.
1. Diet And Lifestyle Factors
One of the most significant contributors to secondary hyperlipidemia is an unhealthy diet and sedentary lifestyle.
Consuming a diet high in saturated fats, trans fats, and cholesterol can elevate blood lipid levels. Foods such as red meat, full-fat dairy products, fried foods, and processed snacks are common culprits. Additionally, excessive alcohol consumption can lead to increased triglycerides.
a. Poor Dietary Choices
Saturated and Trans Fats: These fats, found in animal products and processed foods, can raise low-density lipoprotein (LDL) cholesterol levels, commonly known as “bad” cholesterol.
High Cholesterol Foods: Consuming large amounts of dietary cholesterol, found in foods like egg yolks, shellfish, and organ meats, can contribute to elevated blood cholesterol levels.
Refined Carbohydrates and Sugars: Diets high in refined carbs and sugars can increase triglyceride levels, contributing to hyperlipidemia.
SEE ALSO: What Body System Is Hyperlipidemia?
b. Lack of Physical Activity
Sedentary Lifestyle: Physical inactivity can decrease high-density lipoprotein (HDL) cholesterol, known as “good” cholesterol, and increase triglycerides. Regular exercise helps improve lipid profiles by boosting HDL and lowering LDL and triglycerides.
2. Obesity
Obesity is closely linked with secondary hyperlipidemia. Excess body fat, particularly around the abdomen, is associated with higher levels of LDL cholesterol and triglycerides, and lower levels of HDL cholesterol. The mechanisms behind this include increased production of very low-density lipoprotein (VLDL) by the liver and decreased clearance of triglycerides from the bloodstream.
a. Metabolic Syndrome
Insulin Resistance: Obesity often leads to insulin resistance, a condition where the body’s cells do not respond effectively to insulin.
This can result in increased lipid production and decreased lipid breakdown.
Inflammation: Excess adipose tissue produces inflammatory cytokines that can affect lipid metabolism, further contributing to hyperlipidemia.
3. Medical Conditions
Several medical conditions can lead to secondary hyperlipidemia.
These conditions often disrupt normal lipid metabolism, leading to elevated blood lipid levels.
a. Diabetes Mellitus
Type 2 Diabetes: Insulin resistance and high blood sugar levels in type 2 diabetes can increase triglycerides and lower HDL cholesterol.
Type 1 Diabetes: Poorly controlled type 1 diabetes can also lead to elevated triglycerides and LDL cholesterol levels.
b. Hypothyroidism
Reduced Thyroid Function: Hypothyroidism slows down metabolism, leading to increased levels of total cholesterol and LDL cholesterol.
c. Chronic Kidney Disease
Dyslipidemia: Kidney disease can disrupt lipid metabolism, leading to elevated triglycerides and decreased HDL cholesterol.
d. Liver Diseases
Non-Alcoholic Fatty Liver Disease (NAFLD): This condition is often associated with insulin resistance and obesity, leading to elevated triglycerides and LDL cholesterol.
e. Polycystic Ovary Syndrome (PCOS)
Hormonal Imbalance: PCOS can cause insulin resistance and metabolic abnormalities, including dyslipidemia.
4. Medications
Certain medications can alter lipid levels, leading to secondary hyperlipidemia. These medications can either increase lipid production or decrease lipid clearance.
a. Corticosteroids
Increased Lipid Synthesis: Corticosteroids can increase the synthesis of triglycerides and cholesterol in the liver.
b. Anabolic Steroids
Altered Lipid Metabolism: These steroids can reduce HDL cholesterol and increase LDL cholesterol.
c. Beta-Blockers
Impact on Lipids: Beta-blockers, used to treat hypertension and heart disease, can increase triglyceride levels and decrease HDL cholesterol.
d. Thiazide Diuretics
Lipid Elevation: These diuretics can cause modest increases in cholesterol and triglycerides.
e. Oral Contraceptives
Hormonal Influence: Some oral contraceptives can affect lipid metabolism, leading to elevated cholesterol and triglycerides.
5. Smoking And Alcohol Consumption
a. Smoking
Impact on HDL Cholesterol: Smoking is associated with lower levels of HDL cholesterol and increased LDL cholesterol and triglycerides.
Oxidative Stress: Smoking induces oxidative stress, which can damage lipoproteins and promote atherogenesis.
b. Alcohol Consumption
Moderate vs. Excessive Drinking: While moderate alcohol consumption may have a protective effect on HDL cholesterol, excessive drinking can lead to elevated triglycerides and increased risk of hyperlipidemia.
6. Genetic Disorders
While primary hyperlipidemia is primarily genetic, some genetic disorders can also cause secondary hyperlipidemia.
a. Familial Hypercholesterolemia
Genetic Mutation: This disorder is characterized by mutations in the LDL receptor gene, leading to high levels of LDL cholesterol from birth.
b. Familial Combined Hyperlipidemia
Mixed Dyslipidemia: This condition involves elevated levels of LDL cholesterol and triglycerides, often influenced by other secondary factors like obesity and insulin resistance.
7. Hormonal Changes
Hormonal changes, particularly those related to menopause and endocrine disorders, can impact lipid levels.
a. Menopause
Estrogen Decline: The decline in estrogen levels during menopause can lead to increased LDL cholesterol and decreased HDL cholesterol.
b. Cushing’s Syndrome
Cortisol Excess: This condition, characterized by excessive cortisol production, can increase lipid levels.
Management And Treatment
Effective management of secondary hyperlipidemia involves addressing the underlying causes. Lifestyle modifications, such as adopting a heart-healthy diet, regular physical activity, and weight management, are crucial. Additionally, managing medical conditions like diabetes, hypothyroidism, and kidney disease through appropriate medications and treatments can help control lipid levels.
a. Lifestyle Changes
Dietary Adjustments: Reducing intake of saturated and trans fats, refined carbohydrates, and sugars while increasing consumption of fiber-rich foods, fruits, and vegetables.
Exercise: Engaging in regular physical activity to improve lipid profiles.
b. Medical Treatment
Medications: Statins, fibrates, and other lipid-lowering medications may be prescribed to manage lipid levels.
Disease Management: Proper management of underlying conditions like diabetes and hypothyroidism.
c. Avoiding Risk Factors
Smoking Cessation: Quitting smoking to improve HDL cholesterol and reduce LDL cholesterol and triglycerides.
Alcohol Moderation: Limiting alcohol intake to recommended levels.
Conclusion
Understanding the secondary causes of hyperlipidemia is essential for effective management and treatment. By addressing the underlying factors, such as diet, lifestyle, medical conditions, medications, and hormonal changes, individuals can better control their lipid levels and reduce the risk of cardiovascular disease. Regular monitoring and collaboration with healthcare providers are key to managing this complex condition and maintaining overall health.