Hyperlipidemia, characterized by elevated levels of lipids (fats) in the blood, is a critical health condition that can lead to severe cardiovascular problems if not managed properly. It encompasses various lipid disorders, including high cholesterol and high triglycerides. Proper diagnosis is essential for effective management and prevention of associated health risks.
This article will explore the diagnostic process for hyperlipidemia, with a focus on how it relates to individuals with dental diseases, emphasizing the interconnectedness of overall health.
What Is Hyperlipidemia?
Hyperlipidemia involves an imbalance in lipid levels in the bloodstream. This condition often manifests as:
Hypercholesterolemia: Elevated levels of cholesterol, including LDL (low-density lipoprotein) and sometimes total cholesterol.
Hypertriglyceridemia: Increased levels of triglycerides, another type of fat in the blood.
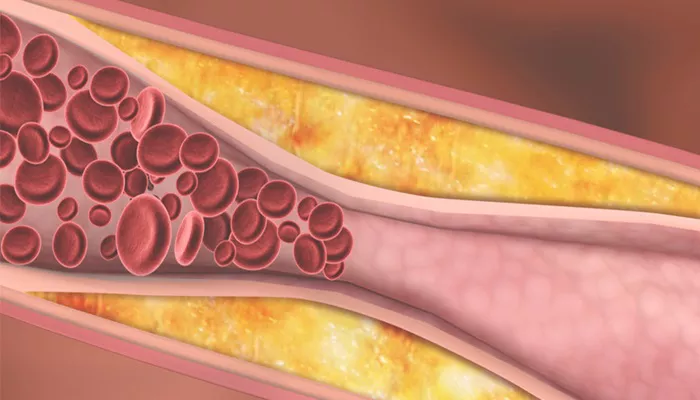
These imbalances can contribute to atherosclerosis (plaque buildup in arteries), increasing the risk of heart disease, stroke, and other cardiovascular issues.
The Diagnostic Process: Step-by-Step
Diagnosing hyperlipidemia involves several steps, starting with identifying risk factors and symptoms, followed by diagnostic testing and evaluation. Here’s a detailed breakdown:
SEE ALSO: The Best 6 Ways to Prevent Hyperlipidemia
1. Identifying Risk Factors
Risk factors for hyperlipidemia include:
Genetics: A family history of lipid disorders.
Lifestyle Factors: Poor diet, lack of exercise, smoking, and excessive alcohol consumption.
Medical Conditions: Diabetes, hypothyroidism, and kidney disease.
Medications: Some drugs can affect lipid levels.
For patients with dental diseases, it’s essential to consider that conditions like periodontal disease can also be associated with systemic health issues, including lipid imbalances. Chronic inflammation from dental diseases may exacerbate hyperlipidemia.
2. Clinical Assessment and Symptoms
During a medical evaluation, the following are considered:
Patient History: A thorough review of the patient’s medical history, family history, and lifestyle factors.
Symptoms: While hyperlipidemia often has no symptoms, some individuals might experience signs related to advanced conditions, such as chest pain or signs of cardiovascular disease.
3. Diagnostic Testing
a. Lipid Panel
The cornerstone of diagnosing hyperlipidemia is the lipid panel, a blood test that measures:
Total Cholesterol: The sum of LDL, HDL (high-density lipoprotein), and other lipid components.
LDL Cholesterol: Often termed “bad” cholesterol; high levels are associated with increased risk of heart disease.
HDL Cholesterol: Known as “good” cholesterol; higher levels are protective against heart disease.
Triglycerides: Elevated levels can also contribute to cardiovascular risk.
A standard lipid panel requires fasting for 9-12 hours before the test to ensure accurate measurement of triglycerides and other lipid components.
b. Additional Tests
In some cases, additional tests may be performed:
Lipoprotein(a) Testing: Measures a specific type of lipoprotein associated with cardiovascular risk.
Apolipoprotein B (ApoB) Testing: Assesses the number of LDL particles, providing further insight into cardiovascular risk.
Genetic Testing: For individuals with a family history of lipid disorders, genetic testing may identify inherited conditions like familial hypercholesterolemia.
4. Evaluating Results
After the tests are conducted, results are interpreted to determine the presence and severity of hyperlipidemia:
Normal Levels: Total cholesterol under 200 mg/dL, LDL under 100 mg/dL, HDL 60 mg/dL or higher, and triglycerides under 150 mg/dL.
Borderline High: Total cholesterol between 200-239 mg/dL, LDL 100-129 mg/dL, HDL less than 40 mg/dL, and triglycerides 150-199 mg/dL.
High: Total cholesterol 240 mg/dL or higher, LDL 130 mg/dL or higher, HDL less than 40 mg/dL, and triglycerides 200 mg/dL or higher.
5. Correlation with Dental Health
For patients with dental diseases, it’s important to note the potential link between periodontal disease and hyperlipidemia.
Research suggests that chronic inflammation from periodontal disease can influence lipid levels and exacerbate hyperlipidemia. Therefore, managing dental health is crucial for overall cardiovascular health.
6. Diagnosis and Management Plan
Once hyperlipidemia is diagnosed, a comprehensive management plan is developed, including:
Lifestyle Modifications: Diet changes, regular exercise, weight management, smoking cessation, and moderating alcohol intake.
Medications: Statins, fibrates, niacin, and other lipid-altering drugs may be prescribed depending on lipid levels and individual risk factors.
Regular Monitoring: Ongoing assessment of lipid levels to track the effectiveness of treatment and make adjustments as needed.
Conclusion
Diagnosing hyperlipidemia involves a multifaceted approach, integrating risk factor assessment, diagnostic testing, and ongoing management. For individuals with dental diseases, addressing oral health is an essential component of a holistic approach to managing hyperlipidemia and overall cardiovascular health. By understanding the interconnectedness of systemic health and dental care, patients can better manage their lipid levels and reduce their risk of associated health issues.