Stents are widely used medical devices designed to treat coronary artery disease (CAD) by opening blocked or narrowed arteries. This procedure, known as angioplasty, aims to restore proper blood flow to the heart, which is essential for its function. Although stents significantly improve the quality of life for many individuals with heart conditions, they have been associated with certain risks and complications. One of the potential concerns is whether stents can cause arrhythmia, a condition where the heart beats too fast, too slow, or irregularly.
In this article, we will explore how stents function, their potential connection to arrhythmia, the mechanisms involved, and the treatment methods for managing any arrhythmia that might occur post-stent placement. We will break down the information in a way that is easy to understand, as well as provide a comprehensive overview of potential risks and effective treatment options.
What Is A Stent?
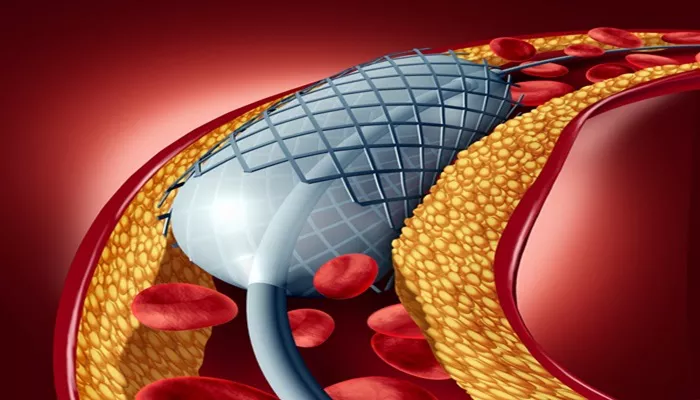
A stent is a small, mesh-like tube inserted into a narrowed or blocked artery to help keep it open and improve blood flow. Stents are primarily used in the coronary arteries, which supply blood to the heart. By restoring proper blood flow, stents help reduce the risk of heart attacks and other serious cardiovascular events. They come in different types, such as bare-metal stents (BMS) and drug-eluting stents (DES), which release medication to prevent the artery from becoming blocked again.
How Do Stents Work?
Stents are typically placed during a procedure called percutaneous coronary intervention (PCI). In this procedure, a balloon catheter is inserted into the artery to widen it, and a stent is deployed to hold the artery open. The stent remains in place permanently, supporting the artery and preventing it from collapsing or narrowing again.
By improving blood flow, stents help deliver oxygen-rich blood to the heart muscle, preventing ischemia (lack of oxygen) that can lead to chest pain (angina) and other severe heart problems.
Can Stents Cause Arrhythmia?
While stents are beneficial in treating coronary artery disease, their use can sometimes trigger arrhythmias, or abnormal heart rhythms.
Arrhythmias can develop immediately after stent placement or even months to years later.
Several factors may contribute to the development of arrhythmias after stent insertion, including:
1. Mechanical Disruption
When a stent is placed, it can sometimes cause mechanical disruption to the artery wall or surrounding tissues. This disruption may lead to abnormal electrical activity in the heart, resulting in arrhythmias. For example, irritation of the coronary artery wall could lead to ventricular arrhythmias, such as ventricular tachycardia or fibrillation.
2. Coronary Artery Spasm
Occasionally, the stented artery may experience a spasm, which is a temporary narrowing or tightening of the artery. This can lead to an inadequate supply of oxygen to the heart muscle and trigger arrhythmias, particularly in the early post-procedure period.
3. Late Stent Thrombosis
Late stent thrombosis is a rare but serious complication that occurs when a blood clot forms in the stent months or years after the procedure. This clot can block blood flow, causing a heart attack and possibly triggering arrhythmias. It is more common with bare-metal stents than drug-eluting stents, but both types can be affected.
4. Scar Tissue Formation
In some cases, scar tissue forms around the stent after it has been placed in the artery. This scarring can interfere with the heart’s normal electrical conduction system and may lead to arrhythmias.
5. Pre-existing Heart Conditions
Patients who undergo stent placement often have pre-existing heart conditions, such as heart failure or previous myocardial infarctions (heart attacks), which increase the risk of developing arrhythmias. These conditions can make the heart more susceptible to abnormal rhythms, especially during periods of stress or after the procedure.
Types of Arrhythmias Caused by Stents
There are several types of arrhythmias that can occur after stent placement. These include:
1. Atrial Fibrillation (AF)
Atrial fibrillation is a common arrhythmia characterized by irregular and often rapid heartbeats originating in the atria (the upper chambers of the heart). It may develop in patients after stent placement due to changes in the heart’s electrical system or stress caused by the procedure.
2. Ventricular Tachycardia (VT)
Ventricular tachycardia is a fast heart rate originating from the ventricles (lower chambers of the heart). This arrhythmia can be triggered by mechanical disruptions or ischemia following stent placement.
3. Ventricular Fibrillation (VF)
Ventricular fibrillation is a life-threatening arrhythmia where the heart quivers instead of beating effectively. This can occur due to severe coronary artery disruption, especially in the setting of stent thrombosis or a heart attack.
4. Bradycardia
Bradycardia, or an abnormally slow heart rate, can occur after stent placement due to damage to the heart’s electrical system during the procedure.
Treatment for Arrhythmias Caused by Stents
The treatment for arrhythmias after stent placement depends on the type of arrhythmia, its severity, and the patient’s overall health. Treatment strategies include:
1. Medications
Antiarrhythmic Drugs: Medications like amiodarone or beta-blockers are often prescribed to control abnormal heart rhythms.
Anticoagulants and Antiplatelets: If stent thrombosis is suspected, medications such as aspirin, clopidogrel, or more potent antiplatelet agents may be given to prevent further clot formation.
Calcium Channel Blockers or Beta-blockers: These drugs can help control the heart rate, especially in cases of atrial fibrillation or tachycardia.
2. Cardioversion
For patients with atrial fibrillation or other fast arrhythmias, electrical cardioversion may be required to reset the heart’s rhythm to normal.
This procedure involves delivering a shock to the heart under controlled conditions.
3. Ablation Therapy
In cases of persistent arrhythmias, such as atrial fibrillation or ventricular tachycardia, catheter ablation may be performed.
This procedure uses radiofrequency energy to destroy small areas of heart tissue that are causing the abnormal rhythms.
4. Implantable Devices
For patients with severe or life-threatening arrhythmias, implantable devices like a pacemaker or implantable cardioverter defibrillator (ICD) may be necessary. These devices help regulate heart rhythm and can deliver shocks if a dangerous arrhythmia occurs.
5. Lifestyle Modifications
Patients are often advised to make lifestyle changes, such as reducing stress, avoiding excessive alcohol or caffeine intake, and engaging in regular physical activity to help manage arrhythmias.
6. Surgical Intervention
In rare cases, surgery may be required to treat arrhythmias, particularly if other treatment options are unsuccessful. This could include bypass surgery or more invasive procedures to address structural heart issues.
Conclusion
While stents are effective in treating coronary artery disease and improving heart function, they can sometimes cause arrhythmias as a complication. The risk of arrhythmia varies depending on several factors, including the type of stent, the patient’s heart condition, and the procedure itself. Understanding the mechanisms behind arrhythmias and recognizing the symptoms early is crucial for managing this potential complication.
Treatment options for arrhythmias after stent placement range from medications to more invasive procedures such as catheter ablation or the implantation of a pacemaker. If you have recently undergone stent placement or are considering the procedure, it’s essential to discuss the risks and benefits with your cardiologist to ensure the best possible outcome for your heart health.
Related topics: