Heart failure (HF) is a complex clinical syndrome resulting from structural or functional impairments of ventricular filling or ejection of blood. The condition is characterized by insufficient blood flow to meet the body’s needs, leading to various systemic and organ-specific manifestations. Among these, cerebrovascular manifestations are particularly significant due to the brain’s critical dependence on a steady blood supply. The relationship between heart failure and cerebrovascular events is multifaceted, involving both direct and indirect mechanisms that contribute to an increased risk of stroke and other neurological complications.
Understanding Heart Failure And Its Systemic Impact
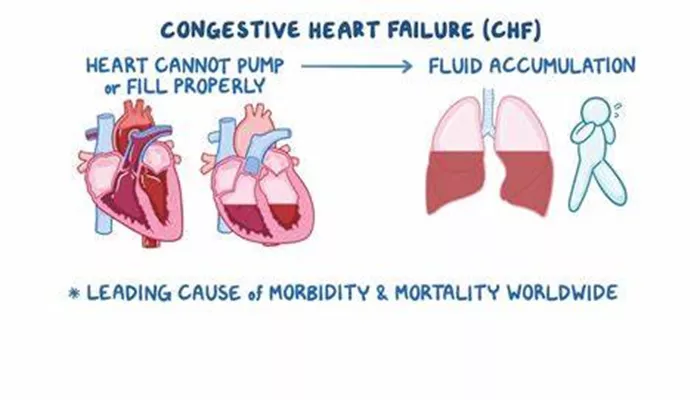
Heart failure can be classified into several types, including systolic heart failure (heart failure with reduced ejection fraction – HFrEF) and diastolic heart failure (heart failure with preserved ejection fraction – HFpEF). Both forms of HF can lead to insufficient cardiac output, which in turn affects the perfusion of vital organs, including the brain. The systemic effects of heart failure include congestion of peripheral tissues, pulmonary edema, and reduced kidney function, all of which can further exacerbate cerebral perfusion issues.
Cerebrovascular events, such as stroke, transient ischemic attacks (TIA), and cognitive impairments, are common in patients with heart failure. These events significantly contribute to morbidity and mortality in this population, making it essential to understand the cerebrovascular manifestations of heart failure to manage and potentially prevent these complications.
Mechanisms Linking Heart Failure to Cerebrovascular Events
The cerebrovascular manifestations of heart failure are primarily due to a combination of hemodynamic changes, neurohormonal activation, and the prothrombotic state associated with HF.
Hemodynamic Changes
Reduced Cardiac Output: Heart failure leads to a decrease in cardiac output, resulting in inadequate cerebral perfusion.
The brain, being highly sensitive to oxygen and nutrient deprivation, is particularly vulnerable to this reduced blood flow, which can lead to ischemic strokes.
Atrial Fibrillation (AF): Heart failure often coexists with atrial fibrillation, a common arrhythmia associated with a fivefold increase in stroke risk. AF leads to stasis of blood in the atria, promoting thrombus formation, which can then embolize to the brain, causing ischemic stroke.
SEE ALSO: How Long Does It Take to Die From Heart Failure?
Neurohormonal Activation
Renin-Angiotensin-Aldosterone System (RAAS): Chronic heart failure triggers the activation of the RAAS, which, while initially compensatory, leads to vasoconstriction, sodium retention, and increased blood pressure, all of which contribute to cerebrovascular damage.
Sympathetic Nervous System (SNS) Activation: Increased SNS activity in heart failure raises blood pressure and heart rate, which can lead to hypertensive crises and increased shear stress on cerebral vessels, predisposing them to rupture and hemorrhagic stroke.
Prothrombotic State
Hypercoagulability: Heart failure induces a prothrombotic state characterized by increased platelet aggregation, elevated fibrinogen levels, and reduced fibrinolytic activity. These factors increase the risk of thromboembolic events, including strokes.
Endothelial Dysfunction: Endothelial cells lining blood vessels play a crucial role in maintaining vascular health. In heart failure, endothelial dysfunction is common, leading to a loss of vasodilatory capacity, increased vascular permeability, and a higher risk of thrombosis.
Cerebrovascular Manifestations of Heart Failure
Ischemic Stroke
Ischemic stroke is the most common cerebrovascular manifestation of heart failure. The reduced cardiac output in HF can result in poor cerebral perfusion, particularly in the setting of systemic hypotension or AF. The brain regions most affected are often those located in watershed areas, which are particularly vulnerable to hypoperfusion.
Risk Factors:
Presence of atrial fibrillation
Severe left ventricular dysfunction
High serum natriuretic peptide levels
History of previous stroke or transient ischemic attack
Prevention:
Anticoagulation therapy in patients with AF
Optimal management of heart failure with guideline-directed medical therapy (GDMT)
Control of hypertension and other cardiovascular risk factors
Hemorrhagic Stroke
Hemorrhagic stroke, though less common than ischemic stroke, can occur in patients with heart failure, particularly in the presence of uncontrolled hypertension or anticoagulation therapy. The risk is further heightened by the fragile state of cerebral vessels in the setting of chronic heart failure.
Mechanisms:
Increased arterial pressure due to RAAS and SNS activation
Use of anticoagulants in patients with AF, which may lead to bleeding complications
Prevention:
Careful management of anticoagulation therapy, balancing the risk of stroke with the risk of bleeding
Blood pressure control through lifestyle modifications and medications
Cognitive Impairment and Dementia
Chronic heart failure has been increasingly recognized as a risk factor for cognitive decline and dementia. The mechanisms underlying this association include chronic cerebral hypoperfusion, embolic events from AF, and the systemic inflammatory state associated with HF.
Clinical Features:
Memory impairment
Difficulty in executive functioning
Reduced attention and processing speed
Prevention and Management:
Early detection and management of heart failure and its comorbidities
Cognitive rehabilitation and lifestyle interventions
Regular screening for cognitive decline in patients with chronic heart failure
Transient Ischemic Attack (TIA)
A transient ischemic attack, often called a “mini-stroke,” is a temporary period of symptoms similar to those of a stroke. TIAs are warning signs of future strokes and are more common in patients with heart failure, particularly those with AF.
Symptoms:
Sudden onset of weakness or numbness on one side of the body
Confusion, trouble speaking or understanding speech
Difficulty seeing in one or both eyes
Dizziness, loss of balance, or coordination
Management:
Immediate medical evaluation and initiation of preventive measures
Antithrombotic therapy for stroke prevention
Aggressive management of heart failure and its associated risk factors
Management Strategies for Cerebrovascular Complications in Heart Failure
Managing the cerebrovascular complications of heart failure requires a comprehensive approach that includes both pharmacological and non-pharmacological strategies.
Pharmacological Interventions
Anticoagulation and Antiplatelet Therapy: To reduce the risk of thromboembolic events, especially in patients with AF.
The choice of therapy must be individualized based on the patient’s bleeding risk.
Neurohormonal Modulation: The use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonists can improve heart failure outcomes and reduce the risk of cerebrovascular events by stabilizing blood pressure and reducing neurohormonal activation.
Diuretics and Vasodilators: These help manage fluid overload and reduce the risk of pulmonary congestion, which can further impair cerebral perfusion.
Non-Pharmacological Interventions
Lifestyle Modifications: These include dietary changes, regular physical activity, smoking cessation, and weight management, all of which can help control blood pressure, improve heart function, and reduce the risk of stroke.
Device Therapy: In selected patients, devices such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) can improve cardiac function and reduce the risk of sudden cardiac death, thereby indirectly reducing the risk of cerebrovascular events.
Conclusion
The cerebrovascular manifestations of heart failure are significant contributors to the morbidity and mortality associated with the condition. Ischemic and hemorrhagic strokes, cognitive impairment, and transient ischemic attacks are common in patients with heart failure, driven by a complex interplay of hemodynamic changes, neurohormonal activation, and a prothrombotic state. Effective management of these complications requires a comprehensive approach that includes both pharmacological and non-pharmacological strategies, regular monitoring, and patient education.