Luminal irregularities of the coronary artery are a critical aspect of cardiovascular health that require thorough understanding and timely management. These irregularities often indicate underlying conditions that could lead to severe heart complications if left unaddressed. This article will explore what luminal irregularities in coronary arteries mean, the causes and implications, how they are diagnosed, and the various management strategies available.
What Are Luminal Irregularities of Coronary Arteries?
Luminal irregularities in the coronary arteries refer to any abnormalities or inconsistencies in the inner surface of the arteries that supply blood to the heart muscle. The term “luminal” pertains to the lumen, which is the inner open space of the artery through which blood flows. When this space becomes irregular due to plaques, clots, or other factors, it can disrupt the smooth flow of blood, leading to various cardiovascular problems.
These irregularities can range from mild to severe, with potential consequences including restricted blood flow (ischemia), increased risk of blood clot formation (thrombosis), and in extreme cases, complete blockage of the artery, leading to a heart attack (myocardial infarction).
Causes of Luminal Irregularities in Coronary Arteries
Several factors can contribute to the development of luminal irregularities in coronary arteries. These include:
1. Atherosclerosis
Atherosclerosis is one of the most common causes of luminal irregularities. It occurs when plaque—a mixture of fat, cholesterol, and other substances—builds up on the arterial walls. Over time, these plaques can harden and narrow the lumen, causing irregularities. This condition is often associated with high cholesterol levels, smoking, hypertension, and a sedentary lifestyle.
2. Coronary Artery Disease (CAD)
Coronary Artery Disease is characterized by the narrowing or blockage of coronary arteries due to atherosclerosis. As the plaques accumulate, they cause irregularities in the artery’s lumen, which can lead to reduced blood flow to the heart muscle. CAD is a leading cause of heart attacks and angina (chest pain).
SEE ALSO: What Does Acute Coronary Syndrome Include
3. Inflammation
Inflammatory processes within the arteries can also lead to luminal irregularities. Conditions like vasculitis (inflammation of blood vessels) can damage the endothelial lining of the arteries, leading to swelling, irregularities, and even clot formation. Chronic inflammation is often linked to autoimmune diseases, infections, or prolonged exposure to certain toxins.
4. Thrombosis
The formation of blood clots (thrombi) within the coronary arteries can cause sudden luminal irregularities. When a clot partially or completely obstructs the lumen, it can lead to acute coronary events such as a heart attack. Thrombosis is often triggered by atherosclerotic plaques, irregular heart rhythms (such as atrial fibrillation), or prolonged immobility.
5. Coronary Artery Spasm
A coronary artery spasm, also known as Prinzmetal’s angina, is a temporary constriction of the coronary artery that can cause luminal irregularities. This spasm can reduce or completely block blood flow to the heart, leading to chest pain or even a heart attack if prolonged. The exact cause of coronary artery spasms is not fully understood, but they are often associated with smoking, stress, and the use of certain drugs like cocaine.
6. Congenital Abnormalities
Some individuals are born with congenital abnormalities in the structure of their coronary arteries, leading to luminal irregularities. These abnormalities can affect the size, shape, or position of the arteries, potentially leading to compromised blood flow and an increased risk of cardiovascular events.
7. Medical Procedures and Trauma
Luminal irregularities can also occur as a result of medical procedures or trauma. For example, coronary angioplasty—a procedure to widen narrowed arteries—can sometimes cause damage to the arterial walls, leading to irregularities.
Similarly, blunt chest trauma or injury from invasive procedures like catheterization can disrupt the smooth lining of the coronary arteries.
Implications of Luminal Irregularities in Coronary Arteries
The presence of luminal irregularities in coronary arteries has significant implications for cardiovascular health. These irregularities can lead to a range of complications, depending on their severity and underlying cause.
1. Reduced Blood Flow (Ischemia)
One of the most immediate implications of luminal irregularities is reduced blood flow to the heart muscle, a condition known as ischemia. When the lumen of the coronary artery is narrowed or obstructed, it limits the amount of oxygen-rich blood that reaches the heart. Ischemia can lead to symptoms like chest pain (angina), shortness of breath, and fatigue, particularly during physical activity.
2. Increased Risk of Heart Attack (Myocardial Infarction)
Severe luminal irregularities, especially those caused by atherosclerosis or thrombosis, can lead to a complete blockage of the coronary artery. When the blood flow is entirely cut off, it results in a heart attack (myocardial infarction). This condition requires immediate medical attention to restore blood flow and minimize heart damage.
3. Arrhythmias
Irregular blood flow caused by luminal irregularities can also lead to arrhythmias, or irregular heart rhythms. When the heart muscle is deprived of adequate blood supply, it can cause electrical disturbances in the heart, leading to conditions such as atrial fibrillation, ventricular tachycardia, or even sudden cardiac arrest.
4. Heart Failure
Over time, chronic luminal irregularities can contribute to heart failure, a condition where the heart is unable to pump blood effectively. Persistent ischemia and recurrent heart attacks can weaken the heart muscle, leading to reduced cardiac output and symptoms like swelling in the legs, fatigue, and shortness of breath.
5. Angina
Angina is a common symptom of luminal irregularities, particularly in cases of coronary artery disease. It manifests as chest pain or discomfort due to reduced blood flow to the heart muscle. Angina can be stable, occurring during physical exertion, or unstable, occurring unexpectedly and often signaling an impending heart attack.
Diagnosis of Luminal Irregularities in Coronary Arteries
The diagnosis of luminal irregularities in coronary arteries involves a combination of clinical evaluation, imaging studies, and sometimes invasive procedures. Early diagnosis is crucial for effective management and prevention of serious cardiovascular events.
1. Clinical Evaluation
The first step in diagnosing luminal irregularities is a thorough clinical evaluation. This includes a detailed medical history, assessment of risk factors (such as hypertension, diabetes, smoking, and family history of heart disease), and physical examination. Symptoms like chest pain, shortness of breath, and fatigue are carefully evaluated.
2. Electrocardiogram (ECG)
An electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart. It can help identify signs of ischemia, arrhythmias, or a previous heart attack, which may be associated with luminal irregularities.
3. Stress Testing
Stress testing involves monitoring the heart’s function during physical exertion, typically on a treadmill or stationary bike.
It can help identify ischemia caused by luminal irregularities by assessing the heart’s response to increased demand for oxygen.
4. Coronary Angiography
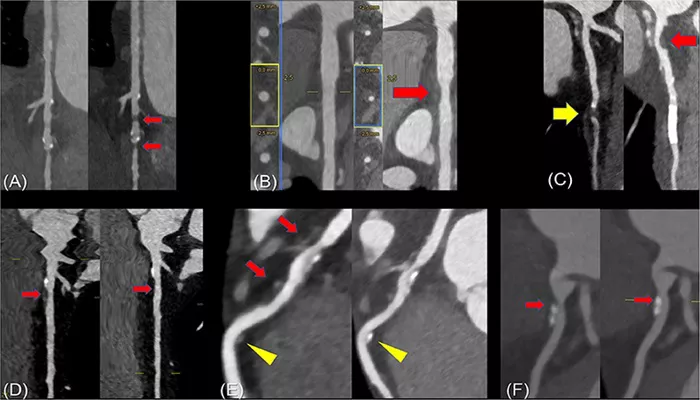
Coronary angiography is the gold standard for diagnosing luminal irregularities in the coronary arteries. This invasive procedure involves injecting a contrast dye into the coronary arteries and taking X-ray images to visualize the lumen.
Angiography can precisely identify the location, extent, and severity of luminal irregularities, such as narrowing or blockages.
5. Intravascular Ultrasound (IVUS)
Intravascular ultrasound (IVUS) is an advanced imaging technique that uses sound waves to create detailed images of the inside of the coronary arteries. IVUS can provide information about the thickness of the arterial walls, the presence of plaques, and the degree of luminal irregularities.
6. Computed Tomography Angiography (CTA)
Computed tomography angiography (CTA) is a non-invasive imaging technique that uses X-rays to create detailed cross-sectional images of the coronary arteries. CTA is particularly useful for visualizing luminal irregularities and assessing the extent of coronary artery disease.
Conclusion
Luminal irregularities of the coronary arteries are a significant concern in cardiovascular health, with potential implications ranging from mild ischemia to life-threatening heart attacks. Understanding the causes, implications, and management strategies for these irregularities is crucial for preventing serious cardiovascular events and improving patient outcomes.
Through a combination of lifestyle modifications, medications, and, when necessary, medical procedures, individuals with luminal irregularities can achieve better heart health and reduce their risk of complications.