Vasodilation is a critical physiological process that plays a significant role in regulating blood pressure. It involves the widening or relaxation of blood vessels, which is primarily mediated by the smooth muscles in the vessel walls. This process can occur in response to various factors, including physical activity, temperature changes, chemical signals, and the body’s need to deliver more oxygen and nutrients to tissues.
To comprehend why vasodilation leads to low blood pressure, it is essential to understand the relationship between blood vessel diameter and blood pressure. Blood pressure is the force exerted by circulating blood on the walls of blood vessels, and it is determined by several factors, including cardiac output (the volume of blood the heart pumps per minute), blood volume, and the resistance offered by blood vessels (peripheral resistance). Vasodilation directly affects the peripheral resistance, which in turn influences blood pressure.
The Mechanics of Blood Pressure Regulation
Blood pressure is regulated by a complex interplay of systems within the body, primarily the autonomic nervous system, the renin-angiotensin-aldosterone system (RAAS), and the kidneys. These systems work together to ensure that blood pressure remains within a healthy range, allowing for adequate perfusion of organs and tissues.
The autonomic nervous system controls the contraction and relaxation of smooth muscle in the blood vessel walls through the sympathetic and parasympathetic branches. The sympathetic nervous system typically induces vasoconstriction, which narrows blood vessels and increases blood pressure. Conversely, the parasympathetic nervous system promotes vasodilation, reducing vascular resistance and thereby lowering blood pressure.
The RAAS, a hormone system, also plays a pivotal role in blood pressure regulation. It adjusts blood pressure by altering blood volume and vessel tone. Angiotensin II, a potent vasoconstrictor, increases blood pressure by narrowing blood vessels.
However, certain conditions and medications can counteract this effect, leading to vasodilation and a subsequent decrease in blood pressure.
SEE ALSO: Why Would Your Blood Pressure Drop Suddenly
The Role of Peripheral Resistance in Blood Pressure
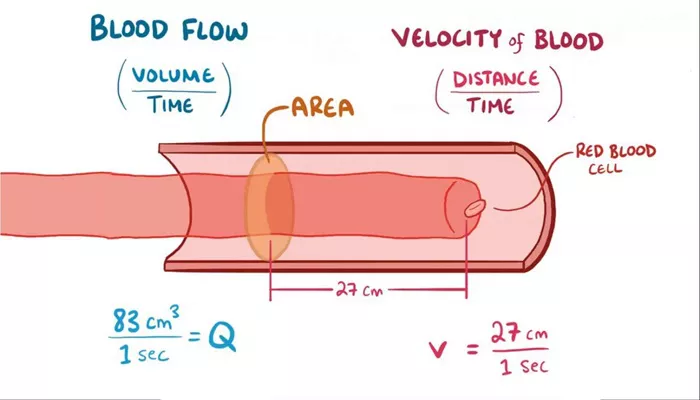
Peripheral resistance refers to the resistance blood encounters as it flows through the circulatory system. This resistance is influenced by factors such as blood vessel diameter, blood viscosity, and the overall length of the circulatory pathway. Of these factors, the diameter of blood vessels is the most dynamic and influential in regulating blood pressure.
When blood vessels constrict (vasoconstriction), the diameter of the vessels decreases, leading to increased resistance to blood flow. This higher resistance causes the heart to work harder to pump blood through the narrowed vessels, resulting in elevated blood pressure. On the other hand, when blood vessels dilate (vasodilation), the diameter increases, reducing resistance and subsequently lowering blood pressure.
How Vasodilation Leads to Low Blood Pressure
Vasodilation leads to low blood pressure through the following mechanisms:
Decreased Peripheral Resistance: As blood vessels dilate, the overall resistance within the circulatory system decreases.
With less resistance, the heart does not need to exert as much force to pump blood through the vessels, leading to a reduction in blood pressure.
Increased Vascular Capacity: When blood vessels widen, they can accommodate a greater volume of blood without an increase in pressure. This increased capacity means that for a given volume of blood, the pressure exerted on the vessel walls is lower, contributing to a drop in blood pressure.
Redistribution of Blood Flow: Vasodilation often occurs in specific regions of the body in response to localized needs, such as increased blood flow to muscles during exercise or to the skin during heat exposure. This targeted dilation can divert blood away from other areas, reducing overall systemic pressure.
Enhanced Venous Return: In some cases, vasodilation can increase the return of blood to the heart by reducing resistance in the venous system. However, if vasodilation is widespread or excessive, it can lead to pooling of blood in the veins, decreasing the effective circulating blood volume and lowering blood pressure.
Physiological And Pathological Causes of Vasodilation
Vasodilation can be induced by several physiological processes as well as pathological conditions. Understanding these causes is crucial for recognizing when vasodilation may lead to clinically significant hypotension.
Physiological Causes
Exercise: During physical activity, vasodilation occurs in the muscles to increase blood flow and oxygen delivery. While this is a normal and beneficial response, it can cause a temporary drop in blood pressure, particularly if the body is not adequately conditioned.
Heat Exposure: Exposure to high temperatures causes vasodilation, especially in the skin, to dissipate heat and regulate body temperature. This process can lead to lower blood pressure, especially if prolonged exposure causes dehydration.
Dietary Factors: Certain foods and nutrients, such as those rich in nitric oxide (e.g., beets, leafy greens), promote vasodilation. Nitric oxide is a potent vasodilator that relaxes the smooth muscles in blood vessels, leading to decreased blood pressure.
Pathological Causes
Sepsis: Sepsis is a severe systemic infection that can lead to widespread vasodilation as part of the body’s inflammatory response. This massive dilation can cause a significant drop in blood pressure, leading to septic shock if not promptly treated.
Anaphylaxis: Anaphylactic reactions involve the release of histamines and other mediators that cause vasodilation. This rapid and extensive dilation can result in a sudden and dangerous drop in blood pressure, requiring immediate medical intervention.
Neurogenic Shock: Neurogenic shock occurs when there is a disruption in the autonomic nervous system, often due to spinal cord injury. This disruption can lead to unopposed parasympathetic activity, causing widespread vasodilation and hypotension.
Medications: Certain medications, such as antihypertensives (e.g., ACE inhibitors, calcium channel blockers), nitrates, and some anesthetics, induce vasodilation as a therapeutic effect. While beneficial in treating hypertension or angina, these drugs can also cause excessive drops in blood pressure if not carefully monitored.
Clinical Implications of Vasodilation-Induced Hypotension
While vasodilation is a natural and necessary process, excessive or inappropriate vasodilation can lead to hypotension, with potentially serious consequences. Low blood pressure can result in inadequate perfusion of vital organs, leading to symptoms such as dizziness, fainting, and, in severe cases, organ damage due to ischemia.
Symptoms of Low Blood Pressure
Dizziness and Lightheadedness: These are common symptoms of low blood pressure, particularly when standing up quickly (orthostatic hypotension). They result from reduced blood flow to the brain.
Fatigue and Weakness: Prolonged low blood pressure can lead to feelings of fatigue and general weakness, as the body’s tissues receive less oxygen and nutrients.
Blurred Vision: Insufficient blood flow to the eyes can cause visual disturbances, including blurred vision.
Fainting (Syncope): In severe cases, low blood pressure can lead to fainting, particularly in situations where blood flow to the brain is significantly compromised.
Shock: If blood pressure drops too low, it can lead to shock, a life-threatening condition characterized by poor organ perfusion and the potential for organ failure.
Management of Vasodilation-Induced Hypotension
The management of low blood pressure due to vasodilation depends on the underlying cause. In some cases, no treatment is necessary, and the condition is self-limiting. However, when hypotension is symptomatic or potentially dangerous, interventions may be required.
Fluid Resuscitation: In cases where hypotension is due to dehydration or blood loss, intravenous fluids can help restore blood volume and increase blood pressure.
Vasoconstrictors: In emergencies, medications that induce vasoconstriction may be used to counteract excessive vasodilation and raise blood pressure.
Addressing Underlying Causes: Treating the root cause of vasodilation, such as infections in sepsis or allergic reactions in anaphylaxis, is crucial for stabilizing blood pressure.
Medication Adjustment: If hypotension is drug-induced, adjusting the dosage or switching to alternative medications may be necessary.
Conclusion
Vasodilation is a fundamental physiological process that plays a critical role in regulating blood pressure and ensuring adequate blood flow to tissues. However, when vasodilation is excessive or occurs under certain pathological conditions, it can lead to low blood pressure, with potentially serious consequences.