Hyperlipidemia, characterized by elevated levels of lipids (fats) in the blood, is a major risk factor for cardiovascular diseases such as coronary artery disease, stroke, and peripheral artery disease. The condition often presents asymptomatically, making early detection crucial for effective management and prevention of related complications. Screening for hyperlipidemia allows for the identification of individuals at risk and provides an opportunity for early intervention to reduce long-term health risks.
In this article, we will explore the recommended guidelines and best practices for screening for hyperlipidemia. We will discuss the timing of screening, the populations at highest risk, and the methods used for detection, as well as the implications of screening results and subsequent management strategies.
What Is Hyperlipidemia?
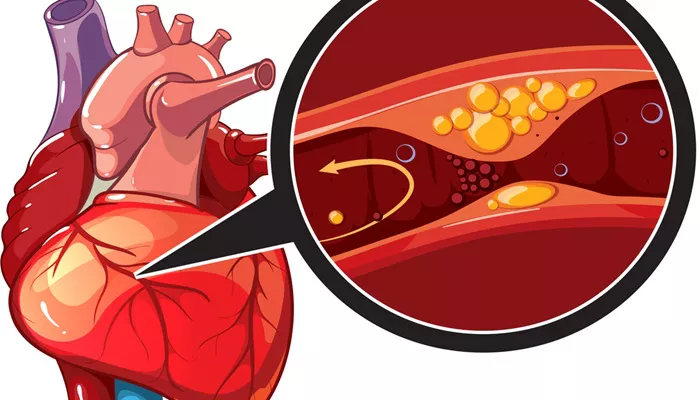
Hyperlipidemia involves elevated levels of lipids in the blood, primarily cholesterol and triglycerides. Cholesterol is carried in the blood by lipoproteins, which include low-density lipoprotein (LDL) and high-density lipoprotein (HDL). Elevated LDL cholesterol, often referred to as “bad” cholesterol, is associated with an increased risk of atherosclerosis and cardiovascular events. Conversely, HDL cholesterol, known as “good” cholesterol, helps to remove excess cholesterol from the bloodstream, providing a protective effect against heart disease.
Triglycerides are another type of lipid found in the blood. High levels of triglycerides are associated with an increased risk of cardiovascular diseases and may also indicate metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes.
SEE ALSO: How Does Hyperlipidemia Cause Atherosclerosis?
Why Screening for Hyperlipidemia Is Important
Early Detection: Hyperlipidemia often does not cause symptoms, making it difficult to detect without routine screening.
Early detection allows for timely intervention to manage lipid levels and reduce cardiovascular risk.
Preventing Cardiovascular Diseases: Elevated lipid levels are a significant risk factor for atherosclerosis, which can lead to heart attacks, strokes, and other serious cardiovascular conditions. Identifying and managing hyperlipidemia can prevent or delay the onset of these diseases.
Managing Risk Factors: Screening helps identify individuals with elevated lipid levels who may also have other risk factors such as hypertension, diabetes, or a family history of cardiovascular disease. Addressing these risk factors together can improve overall health outcomes.
Guiding Treatment Decisions: Screening results inform healthcare providers about the need for lifestyle changes, medications, or other interventions to manage lipid levels and reduce cardiovascular risk.
Current Screening Guidelines
Screening guidelines for hyperlipidemia have evolved based on emerging evidence and changes in population health trends.
The following are key recommendations from major health organizations regarding when to screen for hyperlipidemia:
1. American College of Cardiology (ACC) and American Heart Association (AHA) Guidelines
Adults Aged 40-75: The ACC/AHA guidelines recommend screening for hyperlipidemia in adults aged 40 to 75 years who are at increased risk for cardiovascular disease. This risk assessment is typically based on factors such as age, sex, blood pressure, smoking status, and diabetes.
Adults Over 75: Screening in adults over 75 years old is individualized, depending on overall health, life expectancy, and the presence of other risk factors. Regular monitoring is recommended for those with a history of cardiovascular disease or other risk factors.
Younger Adults and Adolescents: For individuals younger than 40, screening is generally recommended if there are additional risk factors such as a family history of premature cardiovascular disease, obesity, or diabetes.
2. U.S. Preventive Services Task Force (USPSTF) Guidelines
Adults Aged 40-75 with No History of Cardiovascular Disease: The USPSTF recommends screening for hyperlipidemia in adults aged 40 to 75 years without a history of cardiovascular disease, particularly if they have risk factors such as high blood pressure, diabetes, or are smokers.
Children and Adolescents: The USPSTF recommends selective screening for hyperlipidemia in children and adolescents aged 9 to 11 years and again at 17 to 21 years, especially if there is a family history of early cardiovascular disease or dyslipidemia.
3. National Lipid Association (NLA) Recommendations
Routine Screening: The NLA supports routine screening for hyperlipidemia starting at age 20 and recommends follow-up every 4-6 years for individuals with normal lipid levels. More frequent screening may be necessary for those with abnormal lipid levels or risk factors for cardiovascular disease.
High-Risk Groups: The NLA emphasizes the importance of screening individuals with a family history of hyperlipidemia, premature cardiovascular disease, and those with conditions that increase the risk of lipid abnormalities, such as diabetes and metabolic syndrome.
Timing And Frequency of Screening
The timing and frequency of screening for hyperlipidemia depend on various factors, including age, risk factors, and previous screening results. Here are general recommendations:
Starting Age: Screening for hyperlipidemia should begin in early adulthood, typically around age 20. This initial screening establishes a baseline and helps identify individuals at risk of developing lipid abnormalities early.
Interval Between Screenings: For individuals with normal lipid levels and no significant risk factors, screening every 4-6 years is generally recommended. More frequent screening may be required for those with abnormal results, a family history of cardiovascular disease, or other risk factors.
High-Risk Populations: Individuals with conditions such as diabetes, hypertension, or a family history of cardiovascular disease may require more frequent screenings. The exact frequency should be determined based on individual risk assessments and clinical judgment.
Post-Treatment Monitoring: For individuals undergoing treatment for hyperlipidemia, regular follow-up is necessary to monitor the effectiveness of therapy and make any necessary adjustments. Typically, lipid levels are rechecked 6-12 weeks after initiating or adjusting treatment and then periodically thereafter.
Methods of Screening for Hyperlipidemia
Screening for hyperlipidemia involves measuring lipid levels through blood tests. The most common tests used include:
Lipid Panel: A lipid panel, or lipid profile, measures the levels of various lipids in the blood, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. This test provides a comprehensive overview of an individual’s lipid status and helps guide treatment decisions.
Fasting vs. Non-Fasting: Traditionally, lipid panels were performed after fasting for 9-12 hours to obtain accurate measurements of LDL cholesterol and triglycerides. However, recent research suggests that non-fasting lipid panels can also be effective, especially for routine screening. Fasting may still be recommended for certain situations or if triglyceride levels are particularly high.
Genetic Testing: In some cases, genetic testing may be used to identify familial hyperlipidemia, a genetic disorder that causes extremely high levels of cholesterol and an increased risk of early cardiovascular disease. Genetic testing is generally reserved for individuals with a family history of hyperlipidemia or premature cardiovascular events.
Implications of Screening Results
The results of a lipid panel can guide the management of hyperlipidemia and cardiovascular risk. The interpretation of these results involves:
Assessing Lipid Levels: Normal lipid levels typically include an LDL cholesterol level less than 100 mg/dL, an HDL cholesterol level greater than 40 mg/dL for men and 50 mg/dL for women, and triglycerides less than 150 mg/dL. Elevated levels of LDL cholesterol and triglycerides, and low levels of HDL cholesterol, are associated with increased cardiovascular risk.
Risk Assessment: Screening results should be interpreted in the context of other cardiovascular risk factors, such as age, blood pressure, smoking status, and diabetes. Tools like the ASCVD (Atherosclerotic Cardiovascular Disease) risk calculator can help estimate an individual’s 10-year risk of cardiovascular events based on lipid levels and other factors.
Treatment Recommendations: Based on screening results and risk assessment, healthcare providers may recommend lifestyle changes, such as dietary modifications, increased physical activity, and weight management. For individuals with elevated lipid levels or significant cardiovascular risk, pharmacologic treatments such as statins or other lipid-lowering medications may be prescribed.
Conclusion
Screening for hyperlipidemia is a crucial component of cardiovascular disease prevention. By identifying individuals with elevated lipid levels early, healthcare providers can implement effective strategies to manage and reduce cardiovascular risk. Adhering to established guidelines for screening timing and frequency ensures that high-risk individuals receive timely interventions, while routine monitoring helps maintain optimal lipid levels and overall cardiovascular health.