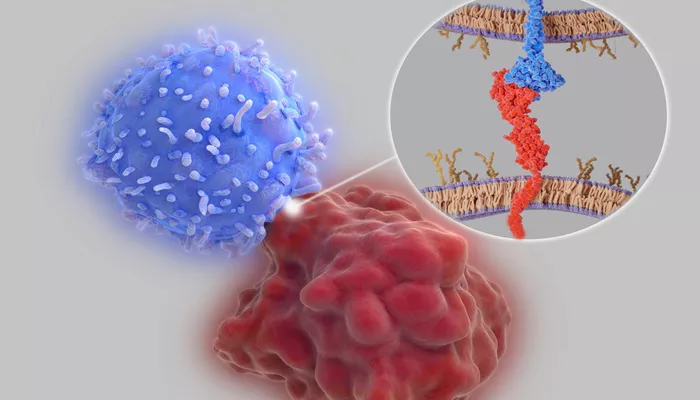
A recent systematic review and meta-analysis has found that while cardiovascular adverse events from immune checkpoint inhibitors (ICIs) are rare in cancer patients, those who develop myocarditis face a significantly higher risk of mortality. Dr. Dorte Lisbet Nielsen, a professor emeritus at the University of Copenhagen, emphasized the importance of recognizing the symptoms and management of this condition.
Background
Immune checkpoint inhibitors have improved treatment outcomes for various cancers. However, they can also lead to immune-related adverse events, particularly affecting the cardiovascular system. These events may include myocarditis, pericarditis, acute coronary syndrome, heart failure, arrhythmias, conduction abnormalities, and cardiac arrest.
“Data on the incidence of cardiotoxicity in the growing number of clinical trials with ICIs are limited,” Dr. Nielsen stated.
This prompted the researchers to systematically gather data and investigate the management of ICI-induced side effects, especially myocarditis.
Research Methodology
Dr. Nielsen and her team conducted two systematic reviews and meta-analyses of studies published up until April 4, 2023.
The first analysis focused on phase 1 to phase 4 trials involving adults with malignant tumors treated with approved ICIs.
The primary endpoint was the incidence of cardiovascular adverse events.
The second analysis included case reports and retrospective studies that examined the clinical manifestations and treatments of patients experiencing ICI-induced cardiovascular events.
Findings on Cardiovascular Events
The first study analyzed data from 83,315 participants across 589 trials. The ICIs included in these trials were pembrolizumab (Keytruda), nivolumab (Opdivo), cemiplimab (Libtayo), atezolizumab (Tecentriq), durvalumab (Imfinzi), avelumab (Bavencio), and ipilimumab (Yervoy).
Results showed that fewer than 1% of patients treated with anti-PD-1 or anti-PD-L1 therapies experienced cardiovascular events (0.8%).
Among these, cemiplimab was linked to a higher risk of severe cardiovascular adverse events (2.91% compared to 0.69% overall).
The study found that 0.24% of patients developed any-grade myocarditis, while 0.2% experienced high-grade myocarditis.
The incidence of cardiovascular events did not significantly differ among patients receiving dual ICI therapy, combination therapy with chemotherapy, or therapy with tyrosine kinase inhibitors. However, those on dual ICI therapy had a notably higher incidence of myocarditis.
Myocarditis Outcomes
In the second analysis, researchers reviewed 223 cases of myocarditis, with 64.5% of the patients being men. Most patients (70%) had received a PD-1 or PD-L1 inhibitor, while 25.6% had dual ICIs, and 4% had ipilimumab.
The analysis revealed that 41.1% of patients had hypertension, 16.3% had diabetes, and 20.9% had no identified risk factors.
Among 220 evaluable patients, the mortality rate for myocarditis was alarmingly high at 37.7%.
Dr. Nielsen remarked, “The mortality rate of myocarditis was much higher than we anticipated.”
Treatment Approaches
Various treatments were used for myocarditis, including:
High-dose corticosteroids: 63.5% showed improvement, but 26% experienced cardiac mortality.
Methylprednisolone (500 to 1,000 mg): 43.5% improved, with a 34.1% cardiac mortality rate.
IV immunoglobulin: 58.7% showed improvement, with a 23.8% cardiac mortality rate.
Plasma exchange: 46.2% improved, with a 26.9% cardiac mortality rate.
Mycophenolate mofetil: 64.4% showed improvement, with a 22.2% cardiac mortality rate.
Infliximab: 38.1% improved, with a 38.1% cardiac mortality rate.
Antithymocyte globulin: 35.3% improved, but 52.9% faced cardiac mortality.
Additionally, 12 patients received abatacept, with 91.7% showing improvement.
The researchers noted that prospective data from 40 patients indicated that systematic screening for respiratory muscle involvement, along with prompt use of abatacept and ruxolitinib, may help reduce mortality rates.