Heart failure is a complex clinical syndrome resulting from the inability of the heart to pump sufficient blood to meet the body’s metabolic demands. Accurate diagnosis is crucial for appropriate management and improved patient outcomes. In this article, we will explore the key diagnostic indicators that help identify heart failure and its underlying causes.
Symptoms And Signs
The initial step in diagnosing heart failure involves assessing the patient’s symptoms and physical examination findings.
Common symptoms include:
Dyspnea: Shortness of breath, particularly with exertion or when lying flat (orthopnea)
Fatigue and weakness: Reduced exercise tolerance and increased tiredness
Edema: Swelling in the legs, ankles, and feet
Cough: Persistent cough or wheezing
Nausea and lack of appetite: Gastrointestinal symptoms due to poor perfusion
Confusion and impaired cognition: Caused by reduced blood flow to the brain
SEE ALSO: What Happens in The End Stage of Heart Failure?
Physical examination may reveal:
Elevated jugular venous pressure: Indicating increased filling pressures
Displaced apical impulse: Suggesting an enlarged heart
S3 heart sound: Presence of a third heart sound, which is a sign of increased ventricular filling pressures
Crackles: Lung crackles or wheezing due to fluid buildup in the lungs
Peripheral edema: Swelling in the legs, ankles, and feet
Hepatomegaly: Enlarged liver due to increased venous pressure
While these symptoms and signs are suggestive of heart failure, they are not specific and may be present in other conditions. Additional tests are necessary to confirm the diagnosis.
Diagnostic Tests
Electrocardiogram (ECG)
An ECG can help identify underlying heart conditions that may contribute to heart failure, such as myocardial infarction, left ventricular hypertrophy, or arrhythmias. However, a normal ECG does not rule out heart failure.
Chest X-ray
A chest X-ray can reveal signs of heart failure, including an enlarged heart, pulmonary congestion, or pleural effusions. It can also help identify other lung diseases that may mimic heart failure symptoms.
Echocardiography
Echocardiography is the most important diagnostic tool for evaluating cardiac structure and function. It can assess left ventricular ejection fraction (LVEF), which is a measure of the heart’s pumping ability. An LVEF below 40% is considered reduced and is characteristic of systolic heart failure.
Echocardiography can also detect other abnormalities, such as valvular heart disease, wall motion abnormalities, and diastolic dysfunction, which may contribute to heart failure.
Biomarkers
Blood tests for natriuretic peptides, such as B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP), can aid in the diagnosis of heart failure. These peptides are released by the ventricles in response to increased wall stress and volume overload.
A normal BNP or NT-proBNP level can effectively rule out heart failure, particularly systolic dysfunction. Elevated levels are more common in systolic heart failure but can also occur in diastolic dysfunction, pulmonary embolism, and other conditions.
Additional Tests
Other tests that may be performed to identify the underlying cause of heart failure include:
Coronary angiography: To assess for coronary artery disease
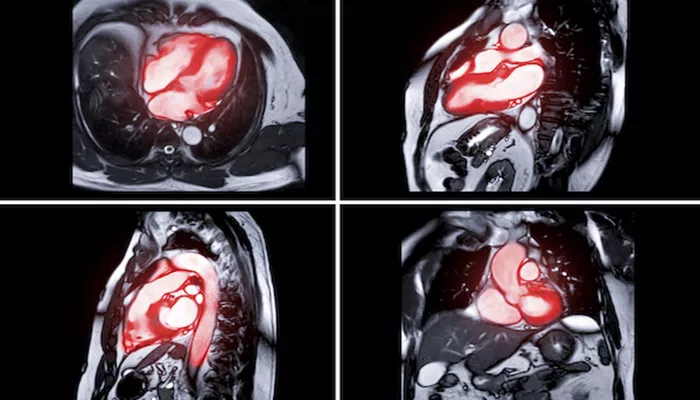
Cardiac magnetic resonance imaging (MRI): To evaluate cardiac structure and function in more detail
Stress testing: To assess for inducible ischemia or exercise capacity
Endomyocardial biopsy: To diagnose specific cardiomyopathies or myocarditis
Diagnostic Criteria
The diagnosis of heart failure requires the presence of both symptoms and objective evidence of cardiac dysfunction. The European Society of Cardiology (ESC) and American College of Cardiology/American Heart Association (ACC/AHA) have proposed diagnostic criteria for heart failure.
According to the ESC, the diagnosis of heart failure requires the following criteria to be met:
Symptoms typical of heart failure (e.g., dyspnea, fatigue, ankle swelling)
Signs typical of heart failure (e.g., elevated jugular venous pressure, pulmonary crackles, peripheral edema)
Objective evidence of a structural or functional cardiac abnormality at rest (e.g., reduced LVEF, elevated natriuretic peptide levels)
The ACC/AHA stages of heart failure provide a framework for the progression of the disease:
Stage A: High risk for developing heart failure but no structural heart disease or symptoms
Stage B: Structural heart disease but no symptoms
Stage C: Structural heart disease with prior or current symptoms
Stage D: Refractory heart failure requiring specialized interventions
Identifying the stage of heart failure helps guide treatment and prognosis.
Differential Diagnosis
Several conditions can mimic or exacerbate the symptoms of heart failure, including:
Chronic obstructive pulmonary disease (COPD): May cause dyspnea and wheezing
Anemia: Can contribute to fatigue and exercise intolerance
Thyroid disorders: May affect heart rate and cardiac function
Obesity: May cause dyspnea and exercise intolerance
It is important to consider these alternative diagnoses and exclude them through appropriate testing.
Conclusion
Diagnosing heart failure requires a comprehensive approach that combines clinical history, physical examination, and diagnostic tests. Key indicators include typical symptoms, signs of volume overload, and objective evidence of cardiac dysfunction. Echocardiography and natriuretic peptide levels are particularly useful in confirming the diagnosis and guiding treatment. By recognizing the diagnostic indicators of heart failure, clinicians can provide timely and appropriate management to improve patient outcomes.