Coronary heart disease (CHD) is a leading cause of morbidity and mortality worldwide. While its impact on the cardiovascular system is well-known, its effects on other systems, particularly the digestive system, are often overlooked.
Understanding how CHD influences the digestive system is essential for comprehensive patient care. This article will delve into the intricate relationship between coronary heart disease and the digestive system, exploring the mechanisms through which CHD can affect digestive function, the symptoms it may cause, and the importance of multidisciplinary management in patients with both cardiovascular and gastrointestinal issues.
The Connection Between Coronary Heart Disease And The Digestive System
Coronary heart disease occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to atherosclerosis. This can lead to myocardial ischemia (reduced blood flow to the heart muscle) and, in severe cases, myocardial infarction (heart attack). While the primary focus of CHD is the heart, the condition can have systemic effects, including on the digestive system.
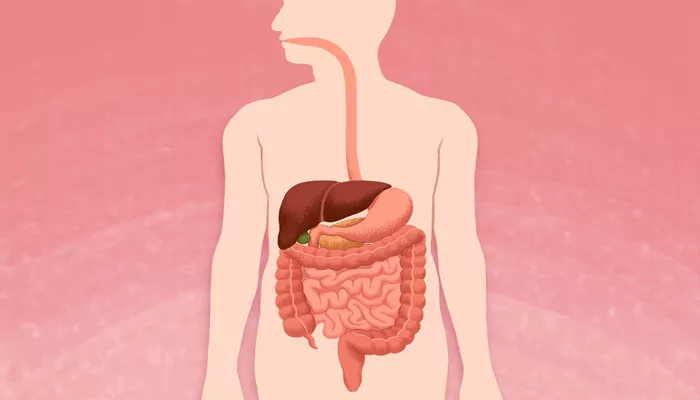
The digestive system, like any other organ system, relies on an adequate blood supply to function properly. The gastrointestinal (GI) tract, which includes the stomach, intestines, liver, and pancreas, requires a steady flow of oxygen-rich blood to maintain its various functions, including digestion, absorption of nutrients, and elimination of waste. When coronary heart disease compromises the cardiovascular system, it can indirectly affect the digestive system through several mechanisms.
SEE ALSO: How Long Can You Live with Cardiac Sarcoidosis?
1. Reduced Blood Flow to the Gastrointestinal Tract
Reduced Blood Flow to the Gastrointestinal Tract
One of the primary ways CHD can affect the digestive system is through reduced blood flow to the gastrointestinal tract.
This can occur for several reasons:
Ischemic Colitis: Ischemic colitis is a condition where the blood flow to the colon is reduced, leading to inflammation and injury. CHD can contribute to ischemic colitis by reducing overall cardiac output, especially during episodes of heart failure or severe ischemia. Symptoms of ischemic colitis include abdominal pain, cramping, and bloody diarrhea. If left untreated, it can lead to severe complications such as bowel necrosis.
Mesenteric Ischemia: Mesenteric ischemia is a condition where the blood flow to the small intestine is reduced. It can be acute or chronic. Acute mesenteric ischemia is a medical emergency and can result from an embolism or thrombosis in the mesenteric arteries. Chronic mesenteric ischemia, often referred to as “intestinal angina,” occurs when atherosclerosis affects the mesenteric arteries, leading to postprandial (after eating) abdominal pain, weight loss, and fear of eating due to the anticipation of pain.
2. Impact of Medications on the Digestive System
Impact of Medications on the Digestive System
Patients with coronary heart disease are often prescribed medications such as antiplatelet agents, anticoagulants, statins, and beta-blockers to manage their condition. While these medications are crucial for cardiovascular health, they can have side effects that impact the digestive system:
Antiplatelet Agents and Anticoagulants: These medications, including aspirin and warfarin, are commonly used to prevent blood clots in CHD patients. However, they can increase the risk of gastrointestinal bleeding, particularly in individuals with a history of peptic ulcers or gastritis. The risk of bleeding is further exacerbated when these medications are combined with nonsteroidal anti-inflammatory drugs (NSAIDs).
Statins: Statins are prescribed to lower cholesterol levels and reduce the risk of heart attacks and strokes. However, they can cause gastrointestinal side effects such as nausea, diarrhea, and abdominal pain. In rare cases, statins can lead to liver dysfunction, which may manifest as jaundice, dark urine, and abdominal discomfort.
Beta-Blockers: Beta-blockers are used to manage high blood pressure and arrhythmias in CHD patients. They can cause gastrointestinal side effects such as constipation, diarrhea, and abdominal cramps. Additionally, beta-blockers may exacerbate symptoms of gastroesophageal reflux disease (GERD) by relaxing the lower esophageal sphincter.
3. Autonomic Dysfunction and Its Effect on Digestive Function
Autonomic Dysfunction and Its Effect on Digestive Function
Coronary heart disease can lead to autonomic dysfunction, a condition where the autonomic nervous system (ANS) does not function properly. The ANS controls involuntary bodily functions, including heart rate, blood pressure, and digestive processes. When the ANS is compromised, it can lead to various gastrointestinal symptoms:
Gastroparesis: Gastroparesis is a condition where the stomach’s ability to empty its contents is delayed. This can lead to symptoms such as nausea, vomiting, bloating, and early satiety. Autonomic dysfunction due to CHD can contribute to gastroparesis by impairing the vagus nerve, which controls stomach motility.
Bowel Dysmotility: The autonomic dysfunction associated with CHD can also affect bowel motility, leading to symptoms such as constipation, diarrhea, or alternating bowel habits. These symptoms can significantly impact a patient’s quality of life and may require careful management to prevent complications such as bowel obstruction or fecal impaction.
4. Heart Failure and Its Impact on the Digestive System
Heart Failure and Its Impact on the Digestive System
Heart failure, a common complication of coronary heart disease, can have a profound impact on the digestive system. When the heart is unable to pump blood effectively, it can lead to congestion in the veins that drain the gastrointestinal organs.
This congestion can cause a range of digestive symptoms:
Hepatic Congestion: Heart failure can lead to congestion in the liver, resulting in hepatomegaly (enlarged liver), ascites (fluid accumulation in the abdomen), and jaundice. Hepatic congestion can also impair liver function, leading to symptoms such as fatigue, nausea, and a decreased ability to metabolize medications.
Intestinal Edema: Heart failure can cause fluid to accumulate in the intestines, leading to intestinal edema. This can impair nutrient absorption and lead to symptoms such as diarrhea, weight loss, and malnutrition. In severe cases, intestinal edema can contribute to bowel ischemia and necrosis.
5. Overlap of Symptoms: Challenges in Diagnosis and Management
Overlap of Symptoms: Challenges in Diagnosis and Management
The overlap of symptoms between coronary heart disease and digestive disorders can pose challenges in diagnosis and management. For example, chest pain is a common symptom of both angina (due to CHD) and gastroesophageal reflux disease (GERD). This overlap can lead to misdiagnosis or delayed diagnosis, potentially resulting in adverse outcomes for the patient.
In some cases, digestive symptoms such as nausea, vomiting, and abdominal pain may be the presenting symptoms of a myocardial infarction, particularly in women, older adults, and individuals with diabetes. It is crucial for healthcare providers to maintain a high index of suspicion and consider the possibility of CHD in patients presenting with atypical symptoms.
Conclusion
Coronary heart disease is a multifaceted condition that can have significant effects on the digestive system. Reduced blood flow, medication side effects, autonomic dysfunction, heart failure, and the overlap of symptoms all contribute to the complex relationship between CHD and gastrointestinal health. By understanding these connections and adopting a multidisciplinary approach to care, healthcare providers can improve the management and outcomes of patients with both coronary heart disease and digestive disorders.