Atrial fibrillation (AFib) is a common heart condition characterized by an irregular and often rapid heartbeat. It occurs when the electrical signals in the heart become chaotic, leading to inefficient pumping of blood. This can result in various symptoms, including palpitations, shortness of breath, and fatigue. AFib is not only uncomfortable but can also increase the risk of serious complications, such as stroke and heart failure. Understanding the causes of AFib is essential for effective management and treatment. This article will explore seven major causes of atrial fibrillation.
What Is Atrial Fibrillation?
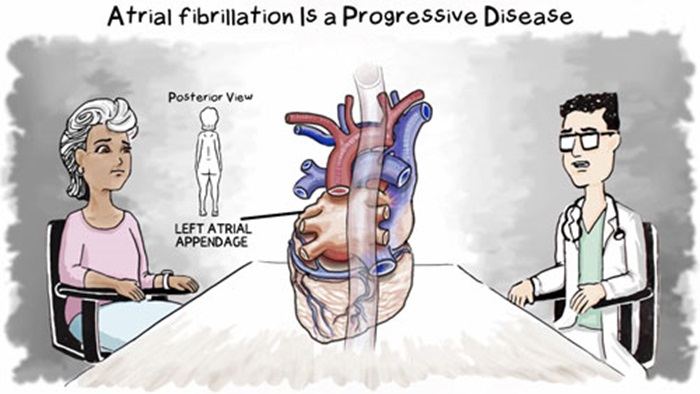
Atrial fibrillation occurs in the heart’s upper chambers, called the atria.
In a healthy heart, electrical signals travel in a coordinated manner, allowing the heart to beat in a regular rhythm. However, in AFib, these signals become disorganized. This results in the atria quivering instead of contracting effectively. As a result, the heart may beat irregularly and rapidly, often exceeding 100 beats per minute.
AFib can manifest in different forms:
Paroxysmal AFib: Episodes come and go, often stopping on their own within 48 hours.
Persistent AFib: Episodes last longer than seven days and may require treatment to restore normal rhythm.
Permanent AFib: The condition is ongoing and does not respond to treatment efforts.
Major Causes of Atrial Fibrillation
Understanding the underlying causes of AFib can help in its prevention and treatment. Here are seven major causes of atrial fibrillation:
1. High Blood Pressure
High blood pressure, or hypertension, is one of the most significant risk factors for developing AFib. When blood pressure is elevated, it puts extra strain on the heart. Over time, this can lead to changes in the heart’s structure, including enlargement of the atria. The enlarged atria can disrupt the normal electrical signals, leading to AFib. Managing blood pressure through lifestyle changes and medication can significantly reduce the risk of developing AFib.
2. Heart Disease
Various forms of heart disease can contribute to the development of AFib. Conditions such as coronary artery disease, heart valve disease, and cardiomyopathy can alter the heart’s structure and function. For example, coronary artery disease can reduce blood flow to the heart muscle, leading to ischemia and scarring. Similarly, heart valve disorders can cause the heart chambers to enlarge, increasing the likelihood of AFib. Regular check-ups and early treatment of heart disease are crucial for preventing AFib.
SEE ALSO: Which Arrhythmia of Are Sawtooth Flutter Waves Characteristic
3. Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions can lead to low oxygen levels and increased pressure in the chest.
Studies have shown that OSA is associated with a higher risk of developing AFib. Treating sleep apnea with lifestyle changes, continuous positive airway pressure (CPAP) therapy, or other interventions can help reduce the risk of AFib.
4. Thyroid Disorders
Thyroid disorders, particularly hyperthyroidism (an overactive thyroid), can trigger AFib. The thyroid gland produces hormones that regulate metabolism and heart function. When the thyroid is overactive, it can lead to an increased heart rate and irregular heart rhythms. Managing thyroid disorders through medication or other treatments can help control heart rhythm and reduce the risk of AFib.
5. Excessive Alcohol Consumption
Excessive alcohol intake is a well-known trigger for AFib. Binge drinking or heavy drinking can lead to episodes of AFib, often referred to as “holiday heart syndrome.” Alcohol can affect the heart’s electrical system and lead to dehydration, both of which can contribute to irregular heartbeats. Reducing alcohol consumption or abstaining altogether can significantly lower the risk of developing AFib.
6. Caffeine and Stimulants
While moderate caffeine consumption is generally safe for most people, excessive intake can lead to palpitations and may trigger AFib in susceptible individuals. Stimulants found in certain medications, energy drinks, and illegal drugs can also provoke AFib episodes.
Individuals who experience AFib should monitor their caffeine intake and avoid stimulants to help manage their condition.
7. Age and Genetic Factors
Age is a significant risk factor for AFib. The likelihood of developing AFib increases as individuals get older, particularly after the age of 65.
Additionally, genetic factors can play a role in the development of AFib.
A family history of AFib or other heart conditions can increase an individual’s risk. While age and genetics cannot be changed, awareness of these factors can help individuals take proactive steps to monitor their heart health.
Symptoms of Atrial Fibrillation
AFib can present with various symptoms, although some individuals may not experience any noticeable symptoms.
Common symptoms include:
Palpitations: A sensation of a racing or fluttering heartbeat.
Shortness of Breath: Difficulty breathing, especially during physical activity or while lying down.
Fatigue: Unusual tiredness or lack of energy.
Dizziness or Lightheadedness: Feeling faint or weak, especially during episodes of rapid heart rate.
Chest Pain: Discomfort or pain in the chest, which may indicate a more serious condition.
Diagnosis of Atrial Fibrillation
If AFib is suspected, a healthcare provider will perform a thorough evaluation, which may include:
Medical History: Discussing symptoms, risk factors, and family history.
Physical Examination: Checking for signs of heart disease or other conditions.
Electrocardiogram (ECG): A test that records the heart’s electrical activity and helps confirm the diagnosis of AFib.
Holter Monitor: A portable device worn for 24-48 hours to monitor heart rhythm continuously.
Echocardiogram: An ultrasound of the heart to assess its structure and function.
Conclusion
Atrial fibrillation is a complex condition with multiple causes, including high blood pressure, heart disease, sleep apnea, thyroid disorders, excessive alcohol consumption, caffeine intake, and genetic factors. Understanding these causes can help individuals take proactive steps to manage their risk and seek appropriate treatment.