Coronary steal syndrome is a complex and intriguing cardiovascular condition characterized by a paradoxical worsening of blood flow to the heart’s already compromised areas. This phenomenon occurs due to the redirection, or “stealing,” of blood from the ischemic regions of the heart to areas with normal or less impaired circulation, leading to exacerbated myocardial ischemia. In this article, we will delve deep into the pathophysiology of coronary steal syndrome, its triggers, clinical presentation, diagnostic approaches, and management strategies, providing a comprehensive overview of what happens in coronary steal syndrome.
The Concept of Coronary Steal
Coronary steal occurs when blood flow is redirected away from the ischemic myocardium to regions with less or no ischemic burden. This usually happens when there is a vasodilatory stimulus, such as the administration of certain pharmacological agents or during stress tests.
When a vasodilator is administered, it causes the normal coronary vessels to dilate, increasing blood flow to regions with healthy arteries. However, the stenotic (narrowed) arteries, already maximally dilated due to their compromised state, cannot respond to this stimulus. The result is that blood is “stolen” from the ischemic areas, where it is most needed, to areas where it is not as critical, worsening the ischemic condition.
Mechanisms Behind Coronary Steal Syndrome
The underlying mechanism of coronary steal syndrome involves the imbalance between myocardial oxygen supply and demand. This imbalance is exacerbated by the differential dilation of coronary vessels during vasodilatory states. Here’s how the process typically unfolds:
Baseline Coronary Flow: Under normal resting conditions, blood flow is relatively evenly distributed across the coronary arteries, with some natural variation depending on the metabolic needs of different myocardial regions.
Vasodilation in Healthy Arteries: When a vasodilator is introduced, the coronary arteries that are not severely stenosed (narrowed) respond by dilating, increasing blood flow to these regions.
Inadequate Response in Stenotic Arteries: The arteries affected by significant stenosis, however, are already maximally dilated due to the chronic ischemic state and cannot further dilate in response to the vasodilator.
Steal Phenomenon: The increased blood flow to the non-stenotic regions “steals” blood away from the areas served by the stenotic arteries, further reducing the oxygen supply to these already compromised myocardial segments.
Exacerbation of Ischemia: The net effect is an exacerbation of ischemia in the areas already suffering from reduced blood flow, potentially leading to angina, arrhythmias, or even myocardial infarction if the ischemia is severe and prolonged.
see also: What Causes Coronary Thrombosis?
Triggers of Coronary Steal Syndrome
Coronary steal syndrome can be triggered by various factors, most commonly during diagnostic or therapeutic procedures involving vasodilators. Understanding these triggers is crucial for the prevention and management of the condition.
Pharmacological Agents
Certain pharmacological agents, particularly vasodilators, are known to precipitate coronary steal syndrome. These include:
Adenosine: Commonly used in myocardial perfusion imaging, adenosine induces coronary vasodilation, which can precipitate coronary steal syndrome in patients with significant coronary artery stenosis.
Dipyridamole: Another vasodilator used in stress testing, dipyridamole can also cause coronary steal by dilating the non-stenotic vessels and diverting blood away from ischemic regions.
Nitroglycerin: Although primarily used to relieve angina by dilating coronary arteries, nitroglycerin can, paradoxically, induce coronary steal in certain cases, particularly when administered in high doses.
Exercise and Physical Stress
Exercise or any form of physical stress increases myocardial oxygen demand. In patients with coronary artery disease, the normal coronary arteries can dilate to meet this demand, while stenotic arteries cannot. This differential response can lead to a similar steal phenomenon as seen with pharmacological vasodilation, exacerbating myocardial ischemia during physical exertion.
Coronary Artery Anomalies
Coronary steal syndrome can also occur in patients with congenital coronary artery anomalies, where abnormal coronary anatomy leads to the diversion of blood flow away from certain myocardial regions. These anomalies, although rare, can significantly impact coronary blood flow dynamics, particularly under stress conditions.
Clinical Presentation of Coronary Steal Syndrome
The clinical presentation of coronary steal syndrome varies depending on the severity of the ischemia and the extent of the underlying coronary artery disease. Common symptoms include:
Angina Pectoris: The most common symptom, angina, manifests as chest pain or discomfort due to myocardial ischemia.
In coronary steal syndrome, angina can occur or worsen during pharmacological stress testing or physical exertion.
Dyspnea: Shortness of breath may accompany angina, especially in cases where ischemia affects a significant portion of the myocardium.
Fatigue and Weakness: These symptoms are often reported by patients during or after physical activity or pharmacological stress tests, reflecting the heart’s reduced ability to meet the body’s increased demands for oxygenated blood.
Arrhythmias: Ischemia can lead to the development of cardiac arrhythmias, ranging from benign palpitations to more severe arrhythmias like ventricular tachycardia or fibrillation, which can be life-threatening.
Silent Ischemia: In some cases, particularly in patients with diabetes or those with a high pain threshold, ischemia may occur without the typical symptoms of angina. This “silent” ischemia can still lead to significant myocardial damage if left untreated.
Diagnostic Approaches to Coronary Steal Syndrome
Diagnosing coronary steal syndrome involves a combination of clinical assessment, imaging studies, and sometimes invasive procedures.
The goal is to identify the presence and extent of coronary artery disease and to assess the risk of coronary steal during diagnostic or therapeutic interventions.
Non-Invasive Imaging
Myocardial Perfusion Imaging (MPI): MPI is commonly used to assess blood flow to the heart muscle during stress and rest.
Vasodilators like adenosine or dipyridamole are often used to induce stress, and areas of reduced perfusion may indicate the presence of coronary steal.
Stress Echocardiography: This test uses ultrasound to visualize the heart’s motion and blood flow during stress, typically induced by exercise or pharmacological agents. Wall motion abnormalities during stress can suggest ischemia and potential coronary steal.
Cardiac Magnetic Resonance Imaging (MRI): MRI provides detailed images of the heart’s structure and function and can be used to assess myocardial perfusion. It is particularly useful in patients who cannot tolerate other forms of stress testing.
Invasive Procedures
Coronary Angiography: This is the gold standard for visualizing the coronary arteries and identifying areas of stenosis.
Angiography can directly demonstrate the presence of significant coronary artery disease, which is necessary for the diagnosis of coronary steal syndrome.
Fractional Flow Reserve (FFR): FFR measures the pressure differences across a coronary stenosis to assess its functional significance. It can help determine whether a particular stenosis is likely to cause ischemia and contribute to coronary steal.
Electrocardiography (ECG)
Exercise Stress Test: An ECG performed during exercise can reveal changes in the heart’s electrical activity that suggest ischemia. This test can indirectly indicate the presence of coronary steal by showing worsening ischemia during physical stress.
Holter Monitoring: Continuous ECG monitoring can detect intermittent ischemia or arrhythmias that may occur during daily activities, providing additional evidence of coronary steal.
Management Strategies for Coronary Steal Syndrome
Managing coronary steal syndrome involves addressing both the underlying coronary artery disease and the specific factors that precipitate the steal phenomenon. Treatment strategies can be broadly categorized into medical management, interventional procedures, and lifestyle modifications.
Interventional Procedures
Percutaneous Coronary Intervention (PCI): Also known as angioplasty, PCI involves the insertion of a stent to open up narrowed coronary arteries. This can relieve the obstruction and reduce the risk of coronary steal by improving blood flow to the ischemic areas.
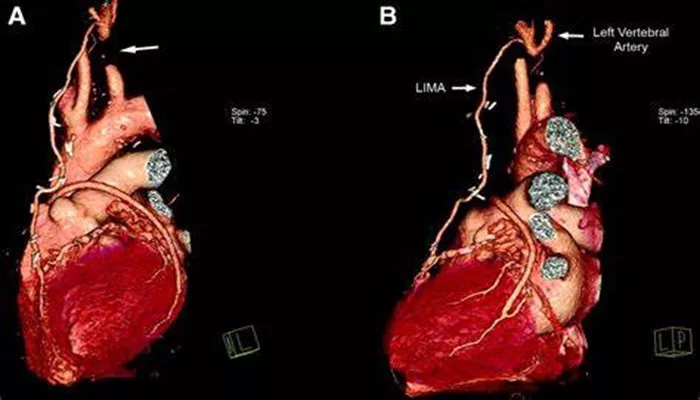
Coronary Artery Bypass Grafting (CABG): In cases of severe or diffuse coronary artery disease, CABG may be necessary. This surgery involves creating a bypass around the blocked coronary arteries using grafts from other vessels, effectively restoring blood flow to the ischemic myocardium.
Lifestyle Modifications
Diet and Exercise: A heart-healthy diet and regular physical activity are crucial in managing coronary artery disease.
Patients should engage in moderate exercise under medical supervision, avoiding activities that could trigger coronary steal.
Smoking Cessation: Smoking is a major risk factor for coronary artery disease, and quitting is essential for reducing the risk of coronary events and improving overall cardiovascular health.
Stress Management: Stress can exacerbate coronary artery disease and contribute to the onset of coronary steal syndrome.
Techniques such as mindfulness, meditation, and relaxation exercises can be beneficial.
Conclusion
Coronary steal syndrome is a complex and potentially dangerous condition that highlights the delicate balance of coronary blood flow. Understanding what happens in coronary steal syndrome is crucial for clinicians to effectively diagnose, manage, and prevent the exacerbation of myocardial ischemia in affected patients.