Embolic strokes are a severe consequence of arrhythmias, particularly those that cause the heart to beat irregularly and inefficiently. Understanding the link between arrhythmias and embolic strokes is crucial for both prevention and treatment.
This article will delve into the most common types of arrhythmias associated with embolic strokes, the mechanisms behind these events, and the importance of early diagnosis and management.
What Is Embolic Strokes?
An embolic stroke occurs when a blood clot or debris travels through the bloodstream and lodges in the brain’s arteries, causing a blockage.
This blockage interrupts the blood flow to the brain, leading to tissue damage and neurological deficits. Unlike thrombotic strokes, which occur due to clots forming directly in the brain’s arteries, embolic strokes originate from other parts of the body, such as the heart, and are then transported to the brain.
The Role of Arrhythmias in Embolic Strokes
Arrhythmias are abnormal heart rhythms that can lead to various complications, including embolic strokes. The irregular heartbeat can cause blood to pool in the heart, leading to the formation of clots. When these clots break free, they can travel to the brain, resulting in an embolic stroke.
SEE ALSO: Which Antidepressant Is Safest for Heart?
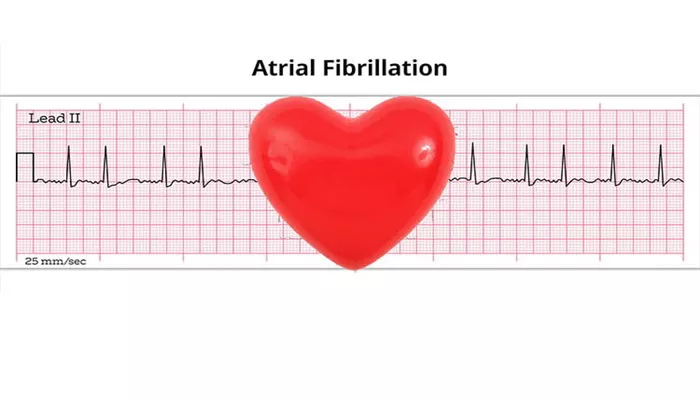
Atrial Fibrillation: The Primary Culprit
Atrial fibrillation (AFib) is the most common arrhythmia implicated in embolic strokes. AFib is characterized by rapid and irregular beating of the atria, the heart’s upper chambers. During AFib, the atria do not contract effectively, causing blood to stagnate and increasing the risk of clot formation.
How Atrial Fibrillation Leads to Embolic Strokes
In AFib, the chaotic electrical activity in the atria prevents them from contracting properly. This inefficiency leads to blood pooling in the left atrium, where it can form clots. If a clot travels from the left atrium to the left ventricle, it can then be pumped into the systemic circulation, potentially lodging in the brain’s arteries and causing an embolic stroke.
Other Arrhythmias Associated with Embolic Strokes
While AFib is the most common arrhythmia associated with embolic strokes, other arrhythmias can also contribute to this risk. These include:
Atrial Flutter
Atrial flutter is similar to AFib but involves a more organized and regular rapid rhythm in the atria. Like AFib, atrial flutter can lead to blood pooling and clot formation, though it is less commonly associated with embolic strokes.
Sick Sinus Syndrome
Sick sinus syndrome (SSS) is a condition where the heart’s natural pacemaker, the sinus node, does not function properly, leading to irregular heartbeats. While SSS itself is less directly linked to embolic strokes, the arrhythmias it causes, such as AFib, increase stroke risk.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a fast heart rhythm originating from the heart’s lower chambers. Although VT is more commonly associated with sudden cardiac death than with embolic strokes, in certain cases, especially when it coexists with AFib, it can increase the risk of clot formation and stroke.
Risk Factors And Prevention
Identifying High-Risk Patients
Certain individuals are at higher risk of developing arrhythmias that can lead to embolic strokes. Risk factors include:
Age: The risk of AFib and related strokes increases with age.
Hypertension: High blood pressure can cause structural changes in the heart, leading to AFib.
Heart Disease: Conditions like heart failure, valvular heart disease, and coronary artery disease increase the risk of arrhythmias.
Diabetes: This condition is associated with a higher risk of both AFib and stroke.
Obesity: Excess weight can contribute to the development of arrhythmias and increase stroke risk.
Preventive Measures
To reduce the risk of embolic strokes in patients with arrhythmias, several preventive strategies can be employed:
Anticoagulation Therapy: Medications like warfarin and newer oral anticoagulants (NOACs) are commonly prescribed to reduce the risk of clot formation in patients with AFib.
Rate and Rhythm Control: Managing the heart rate and rhythm through medications or procedures like cardioversion can help prevent clot formation.
Lifestyle Modifications: Encouraging patients to maintain a healthy weight, control blood pressure, and manage diabetes can reduce the risk of AFib and subsequent strokes.
Diagnosis And Management
Diagnosing Arrhythmias
Early diagnosis of arrhythmias is key to preventing embolic strokes.
Diagnosis typically involves:
Electrocardiogram (ECG): This test records the heart’s electrical activity and can identify irregular rhythms.
Holter Monitor: A portable ECG device worn for 24-48 hours to detect intermittent arrhythmias.
Echocardiogram: This imaging test evaluates the heart’s structure and function, identifying any abnormalities that may contribute to arrhythmias.
Management Strategies
Management of arrhythmias to prevent embolic strokes involves a combination of:
Medications: Antiarrhythmic drugs, beta-blockers, and anticoagulants are commonly used.
Procedures: Cardioversion, catheter ablation, and, in some cases, the implantation of pacemakers or defibrillators may be necessary.
Surgery: In certain cases, surgical intervention, such as the Maze procedure, may be recommended to treat AFib.
Conclusion
Atrial fibrillation is the most common arrhythmia implicated in embolic strokes, with other arrhythmias like atrial flutter and ventricular tachycardia also contributing to this risk. Early diagnosis, effective management, and preventive strategies are crucial in reducing the incidence of embolic strokes in patients with arrhythmias.