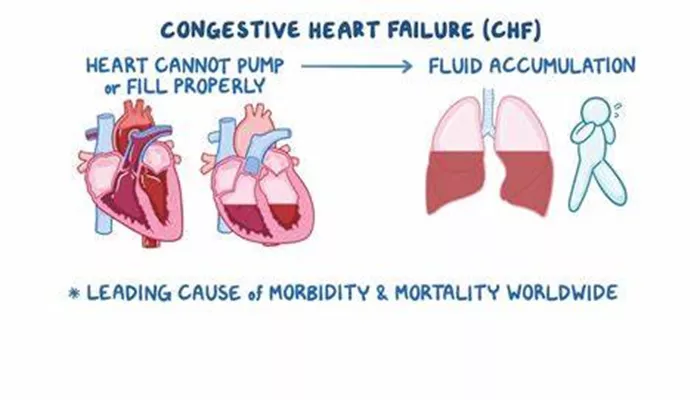
Congestive heart failure (CHF) is a complex medical condition in which the heart cannot pump blood effectively to meet the body’s needs. This condition often leads to symptoms such as shortness of breath, fatigue, and fluid retention. One of the key therapeutic agents used in managing CHF is nitroglycerin. Nitroglycerin, a nitrate drug, plays a significant role in alleviating symptoms and improving the quality of life for patients with CHF.
In this article, we will explore the role of nitroglycerin in the management of congestive heart failure, delving into its mechanisms of action, clinical uses, and potential side effects.
What Is Congestive Heart Failure?
Congestive heart failure occurs when the heart muscle becomes weakened or stiff, impairing its ability to pump blood efficiently. This results in a buildup of fluid in the lungs, legs, and other parts of the body, leading to the characteristic symptoms of CHF. The condition can be caused by various factors, including coronary artery disease, hypertension, valvular heart disease, and cardiomyopathy.
The management of CHF involves a multifaceted approach, including lifestyle changes, medications, and in some cases, surgical interventions. Medications play a crucial role in controlling symptoms, improving heart function, and preventing disease progression.
SEE ALSO: What’s The Main Goal of Compensatory Mechanisms in HF
Mechanism of Action of Nitroglycerin
Nitroglycerin is a vasodilator, meaning it relaxes and widens blood vessels. It primarily acts on the venous system, although it also has effects on the arterial system. The mechanism by which nitroglycerin works can be understood in several key steps:
Conversion to Nitric Oxide: When nitroglycerin enters the body, it is metabolized and converted into nitric oxide (NO).
Nitric oxide is a potent vasodilator that signals the smooth muscles in blood vessels to relax.
Vasodilation of Veins: The primary action of nitroglycerin is the dilation of veins. By widening the veins, nitroglycerin reduces the amount of blood returning to the heart (preload). This decrease in preload reduces the workload on the heart, which is particularly beneficial in CHF, where the heart is already struggling to pump effectively.
Reduction in Myocardial Oxygen Demand: By decreasing preload, nitroglycerin reduces the pressure and volume that the heart must manage, which in turn lowers the heart’s oxygen demand. This is especially important in patients with CHF, where the heart’s oxygen supply is already compromised due to impaired blood flow.
Coronary Artery Dilation: Nitroglycerin also dilates the coronary arteries, improving blood flow to the heart muscle itself.
This is particularly beneficial in patients with CHF who may have underlying coronary artery disease.
Afterload Reduction: Although the effect on arterial vasodilation is less pronounced, nitroglycerin can also reduce afterload (the resistance the heart must overcome to eject blood). This further helps to reduce the stress on the heart.
Clinical Use of Nitroglycerin in Congestive Heart Failure
Acute Decompensated Heart Failure
In acute settings, such as during an episode of acute decompensated heart failure (ADHF), nitroglycerin is often administered intravenously. The rapid onset of action of intravenous nitroglycerin makes it particularly useful in emergencies. It quickly reduces preload and afterload, improving cardiac output and relieving symptoms such as dyspnea (shortness of breath).
Chronic Heart Failure Management
In the chronic management of CHF, nitroglycerin is used in combination with other medications like diuretics, ACE inhibitors, and beta-blockers. Oral or transdermal formulations of nitroglycerin can be used to provide long-term symptom relief. However, due to the development of tolerance with long-term use, nitroglycerin is typically prescribed intermittently or in combination with other nitrates.
Relief of Angina in CHF
Many patients with CHF also suffer from angina due to coronary artery disease. Nitroglycerin is effective in relieving angina by improving coronary blood flow and reducing myocardial oxygen demand. This dual benefit makes nitroglycerin a valuable medication in the management of CHF with concurrent angina.
Side Effects And Considerations
Tolerance Development
One of the significant challenges with nitroglycerin therapy is the development of tolerance. Over time, the body becomes less responsive to the drug, requiring higher doses to achieve the same effect. To prevent tolerance, a nitrate-free interval is often recommended, where the patient stops taking nitroglycerin for a certain period each day.
Hypotension
Nitroglycerin can cause significant hypotension (low blood pressure), especially in patients who are volume-depleted or are on other blood pressure-lowering medications. Hypotension can lead to dizziness, lightheadedness, and in severe cases, syncope (fainting). Therefore, careful monitoring of blood pressure is essential during nitroglycerin therapy.
Headache
Headaches are a common side effect of nitroglycerin due to its vasodilatory effects on the blood vessels in the brain. These headaches are usually mild but can be bothersome for some patients. Over-the-counter pain relievers may be recommended to manage this side effect.
Drug Interactions
Nitroglycerin can interact with several other medications, leading to potentially dangerous effects. For example, the use of nitroglycerin with phosphodiesterase inhibitors (such as sildenafil) can result in severe hypotension. It’s crucial for healthcare providers to review all medications a patient is taking before prescribing nitroglycerin.
Conclusion
Nitroglycerin plays a vital role in the management of congestive heart failure, particularly in reducing the symptoms of acute decompensation and improving the quality of life for patients with chronic CHF. Its ability to reduce preload and afterload, improve coronary blood flow, and alleviate angina makes it a cornerstone in the treatment of CHF. However, the potential for side effects, tolerance development, and drug interactions requires careful patient selection and monitoring.