Heart failure is a complex clinical condition that affects millions of people worldwide. It occurs when the heart cannot pump enough blood to meet the body’s needs for oxygen and nutrients. This inability to circulate blood effectively reduces cardiac output, which is the amount of blood the heart pumps out per minute. Cardiac output is essential for maintaining normal body functions, and its decrease can lead to significant health complications. Understanding how heart failure impacts cardiac output is critical for both managing the condition and improving patients’ quality of life.
What Is Cardiac Output?
Cardiac output refers to the volume of blood the heart pumps per minute. It is calculated by multiplying the heart rate (the number of times the heart beats per minute) by the stroke volume (the amount of blood pumped with each heartbeat). For a healthy adult, normal cardiac output typically ranges between 4 to 8 liters per minute, depending on the individual’s body size, physical activity, and heart function.
The heart’s primary role is to maintain adequate cardiac output to supply oxygen-rich blood to tissues and organs. When cardiac output is compromised, as in heart failure, various systems in the body are affected. These include the kidneys, brain, and muscles, which all rely on a continuous and sufficient blood flow to perform their vital functions.
SEE ALSO: When to Start ACE Inhibitors in Heart Failure?
Heart Failure: A Progressive Condition
Heart failure is often the result of underlying conditions that damage or weaken the heart muscle. Common causes include coronary artery disease, high blood pressure (hypertension), cardiomyopathy (diseases of the heart muscle), heart valve disorders, and previous heart attacks. Over time, these conditions impair the heart’s ability to contract and relax effectively, reducing the heart’s pumping efficiency.
In heart failure, the heart compensates for its reduced ability to pump by enlarging (dilating) to hold more blood, increasing the heart rate, and thickening its walls. However, these compensatory mechanisms are often short-lived, and as the heart becomes more strained, cardiac output declines further.
How Heart Failure Impacts Cardiac Output
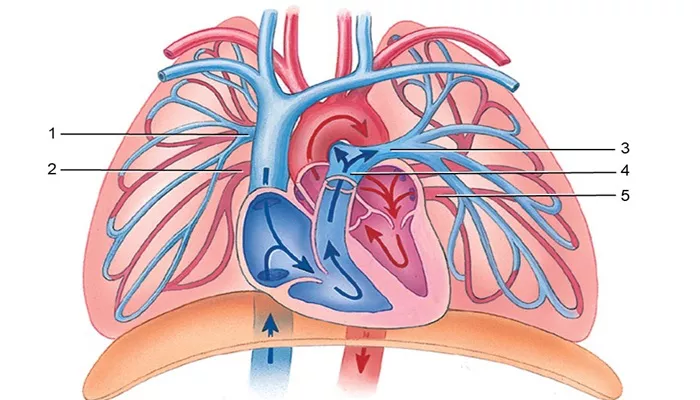
There are two main types of heart failure, and each affects cardiac output in different ways: systolic heart failure (heart failure with reduced ejection fraction) and diastolic heart failure (heart failure with preserved ejection fraction).
1. Systolic Heart Failure and Cardiac Output
Systolic heart failure occurs when the heart’s ability to contract and pump blood is reduced. In this condition, the heart muscle becomes weakened and stretched, leading to a decreased stroke volume. This reduction in stroke volume lowers overall cardiac output.
The key issue in systolic heart failure is the reduced ejection fraction (EF). Ejection fraction is the percentage of blood pumped out of the heart’s left ventricle with each contraction. In a healthy heart, the ejection fraction is typically between 50% and 70%. However, in systolic heart failure, the ejection fraction falls below 40%, meaning that a significant portion of the blood remains in the heart after each beat.
This leads to less blood being circulated to the body, resulting in fatigue, weakness, and shortness of breath.
2. Diastolic Heart Failure and Cardiac Output
In diastolic heart failure, the heart’s pumping ability may remain normal, but its ability to relax and fill with blood between beats is impaired. This happens when the heart muscle becomes stiff or thickened, preventing the left ventricle from filling properly. As a result, the stroke volume decreases, which in turn reduces cardiac output.
Although the ejection fraction may be preserved in diastolic heart failure (typically above 50%), the total volume of blood the heart can pump per beat is reduced. Since less blood enters the heart during the filling phase, less blood is ejected during each contraction, leading to inadequate cardiac output. Patients with diastolic heart failure may experience symptoms such as exercise intolerance, fluid retention, and swelling in the legs or abdomen.
Compensatory Mechanisms And Further Decline
In response to reduced cardiac output, the body activates several compensatory mechanisms to maintain adequate blood flow. These include:
1. Sympathetic Nervous System Activation
The sympathetic nervous system responds to decreased cardiac output by releasing stress hormones such as adrenaline and norepinephrine. These hormones increase the heart rate and contractility in an effort to boost cardiac output. However, over time, chronic activation of the sympathetic nervous system can worsen heart failure by increasing the heart’s workload and oxygen demand.
2. Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is activated in response to reduced blood flow to the kidneys, which occurs when cardiac output is low. This system triggers the release of aldosterone, which causes the body to
retain sodium and water. While this increases blood volume and temporarily boosts cardiac output, it also leads to fluid overload and higher blood pressure. Fluid retention can worsen the symptoms of heart failure, such as swelling (edema) and shortness of breath.
3. Ventricular Remodeling
To compensate for decreased cardiac output, the heart may undergo structural changes, known as ventricular remodeling.
This process includes the thickening (hypertrophy) or dilation of the heart muscle. While remodeling may help maintain cardiac output in the short term, it often leads to further weakening of the heart muscle, increased stiffness, and a continued decline in heart function.
Consequences of Reduced Cardiac Output
Reduced cardiac output has widespread effects on the body’s organs and tissues. Some of the most notable consequences include:
1. Poor Oxygen Delivery
Low cardiac output means that less oxygen-rich blood reaches the body’s organs and tissues. This leads to symptoms such as fatigue, muscle weakness, and reduced exercise capacity. In severe cases, reduced oxygen delivery can cause organ dysfunction, particularly in the kidneys and brain.
2. Fluid Retention
As cardiac output decreases, blood flow to the kidneys is reduced, triggering the RAAS and leading to sodium and water retention. This fluid buildup can cause swelling in the legs, ankles, and abdomen, as well as fluid accumulation in the lungs (pulmonary edema), which leads to shortness of breath and difficulty breathing.
3. Diminished Quality of Life
As heart failure progresses, patients often experience a decline in their ability to perform daily activities due to the reduced cardiac output. Symptoms such as shortness of breath, fatigue, and fluid retention limit physical activity and negatively impact quality of life. Additionally, frequent hospitalizations are common in advanced heart failure, further affecting the patient’s overall well-being.
Treatment Strategies to Improve Cardiac Output
The primary goal in treating heart failure is to improve cardiac output and relieve symptoms. Treatment strategies focus on reducing the heart’s workload, improving its pumping efficiency, and addressing underlying conditions. Common treatments include:
1. Medications
Several classes of medications are used to improve cardiac output in heart failure patients. These include:
ACE inhibitors and ARBs: These drugs reduce the activation of the RAAS, lowering blood pressure and reducing fluid retention.
Beta-blockers: These medications slow the heart rate and reduce the effects of sympathetic nervous system activation, helping to improve cardiac output.
Diuretics: Diuretics help reduce fluid retention, easing the symptoms of fluid overload and improving the heart’s pumping efficiency.
Aldosterone antagonists: These drugs block the effects of aldosterone, reducing fluid retention and preventing further remodeling of the heart muscle.
2. Lifestyle Changes
Patients with heart failure are often advised to make lifestyle changes that can improve cardiac output and overall heart health. These changes include reducing salt intake, maintaining a healthy weight, engaging in moderate exercise, and managing underlying conditions such as high blood pressure or diabetes.
3. Surgical Interventions
In some cases, surgical interventions may be necessary to improve cardiac output. These can include the implantation of a pacemaker, defibrillator, or ventricular assist device (VAD) to support the heart’s function. In severe cases of heart failure, a heart transplant may be the only option to restore normal cardiac output.
Conclusion
Heart failure significantly reduces cardiac output, leading to a range of symptoms and complications that affect the entire body. Whether caused by systolic or diastolic dysfunction, the decline in the heart’s ability to pump blood effectively places a strain on multiple organ systems and reduces quality of life. Understanding the mechanisms behind reduced cardiac output in heart failure allows for targeted treatment strategies that can improve heart function, alleviate symptoms, and enhance patient outcomes.