Supraventricular tachycardia (SVT) is a condition characterized by an abnormally fast heart rate originating above the heart’s ventricles. This condition can occur during various activities, including exercise. Understanding the relationship between exercise and SVT is crucial for patients, athletes, and healthcare providers. This article will explore whether exercise can cause SVT, the mechanisms behind it, and the implications for individuals engaging in physical activity.
Introduction to Supraventricular Tachycardia
SVT is defined as a rapid heart rate exceeding 100 beats per minute, often reaching rates of 150 to 250 beats per minute. It can occur in episodes, sometimes lasting for a few seconds to several hours. While SVT can affect individuals of all ages, it is more common in young adults and those with underlying heart conditions. Symptoms may include palpitations, dizziness, shortness of breath, and chest discomfort.
Understanding The Mechanisms of SVT
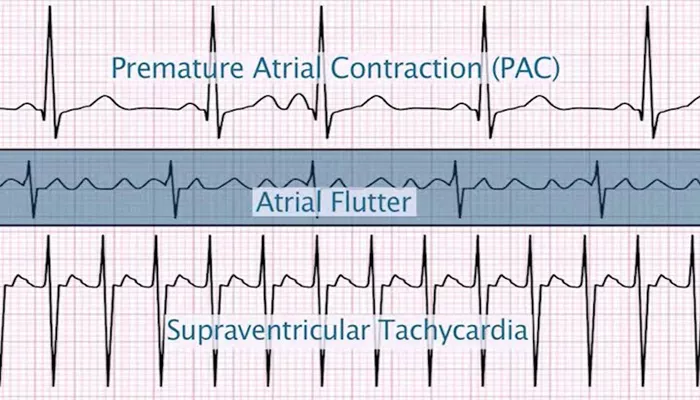
The heart’s electrical system controls its rhythm. When this system malfunctions, it can lead to SVT. There are several types of SVT, including:
Atrial Fibrillation: An irregular and often rapid heart rate that can lead to blood clots.
Atrial Flutter: A fast, regular heartbeat that originates in the atria.
AV Nodal Reentrant Tachycardia (AVRT): A common form of SVT where electrical signals loop back to the atria.
Paroxysmal SVT (PSVT): Episodes of rapid heart rate that start and stop suddenly.
see also: Which Arrhythmia Is Often Implicated with Embolic Strokes
How Exercise Influences SVT
Exercise is known to trigger or exacerbate SVT in some individuals.
During physical activity, the body requires increased blood flow, and the heart rate naturally rises to meet this demand.
However, in susceptible individuals, this increase can lead to the onset of SVT.
Physiological Changes During Exercise
When a person exercises, several physiological changes occur:
Increased Heart Rate: The heart rate increases to supply more oxygen to the muscles. Normal resting heart rates range from 60 to 100 beats per minute, but during intense exercise, this can exceed 180 beats per minute.
Sympathetic Nervous System Activation: Exercise stimulates the sympathetic nervous system, releasing catecholamines like adrenaline, which can increase heart rate and contractility.
Changes in Electrolyte Levels: Physical exertion can alter electrolyte levels in the blood, particularly potassium and magnesium, which are vital for maintaining normal heart rhythm.
Increased Body Temperature: Exercise raises body temperature, which can affect heart function and rhythm.
Evidence Linking Exercise to SVT
Research indicates that exercise can provoke SVT, particularly in individuals with pre-existing conditions. A study published in the American Journal of Cardiology found that exercise-induced SVT occurred in approximately 6% of participants during maximal treadmill testing. Most episodes were short and asymptomatic, often occurring near peak exertion levels.
Another study demonstrated that treadmill exercise tests could reproducibly provoke SVT in patients with a history of exercise-induced episodes. These findings suggest that while exercise can trigger SVT, the majority of cases are not associated with significant cardiovascular risk.
Risk Factors for Exercise-Induced SVT
Several factors can increase the likelihood of experiencing SVT during exercise:
Age: Older individuals may be more susceptible to exercise-induced SVT due to age-related changes in heart structure and function.
Underlying Heart Conditions: Individuals with a history of heart disease, hypertension, or previous episodes of SVT are at higher risk.
Electrolyte Imbalances: Dehydration or imbalances in electrolytes can predispose individuals to arrhythmias during exercise.
Medications: Certain medications that affect heart rate or rhythm may increase the risk of SVT during physical activity.
Excessive Caffeine or Alcohol Intake: Stimulants can exacerbate the likelihood of arrhythmias.
Managing SVT During Exercise
For individuals prone to SVT, managing the condition during exercise is essential. Here are some strategies:
Consult a Healthcare Provider: Individuals with a history of SVT should consult a cardiologist before starting an exercise program. A thorough evaluation can help determine safe exercise levels.
Gradual Warm-Up: A proper warm-up can help prepare the heart for increased activity and may reduce the risk of SVT.
Stay Hydrated: Maintaining proper hydration helps prevent electrolyte imbalances that can trigger SVT.
Monitor Heart Rate: Using a heart rate monitor during exercise can help individuals stay within a safe range and recognize any abnormal increases in heart rate.
Avoid Stimulants: Limiting caffeine and alcohol intake can help reduce the risk of SVT episodes.
Recognize Symptoms: Understanding the symptoms of SVT can help individuals respond quickly if they experience an episode during exercise.
When to Seek Medical Attention
If a person experiences symptoms of SVT during exercise, such as:
A rapid heartbeat that lasts for more than a few minutes
Dizziness or lightheadedness
Chest pain or discomfort
Shortness of breath
They should seek medical attention immediately. In some cases, SVT can lead to more severe complications, especially in individuals with underlying heart conditions.
Conclusion
In summary, exercise can indeed provoke supraventricular tachycardia in some individuals, particularly those with pre-existing conditions or risk factors. While most episodes of exercise-induced SVT are short and asymptomatic, understanding the relationship between exercise and SVT is crucial for individuals at risk.
By taking preventive measures, such as consulting healthcare providers, staying hydrated, and avoiding stimulants, individuals can safely engage in physical activity while minimizing the risk of SVT episodes.