Heart failure (HF) is a significant complication that can arise after a myocardial infarction (MI), commonly known as a heart attack. The development of heart failure after an MI can have serious consequences for a patient’s health and quality of life.
Understanding the causes of heart failure in this context is crucial for prevention, early intervention, and effective management. This article explores the various causes of heart failure following myocardial infarction, providing insights into the underlying mechanisms and risk factors involved.
Introduction to Myocardial Infarction and Heart Failure
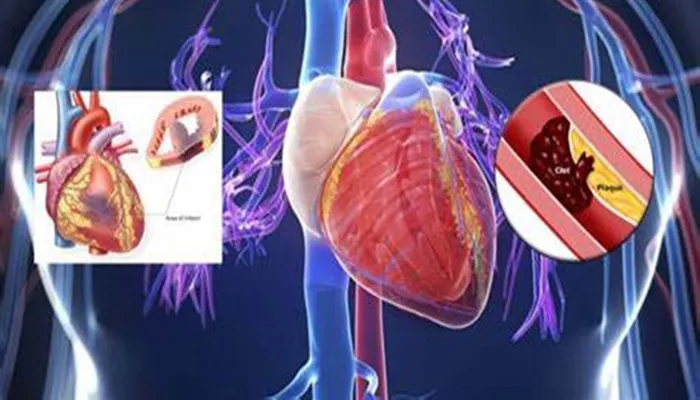
A myocardial infarction occurs when blood flow to a part of the heart is blocked, usually by a blood clot in a coronary artery.
This blockage can cause damage to the heart muscle due to a lack of oxygen. The severity of the damage depends on the duration of the blockage and the size of the affected area.
Heart failure is a condition where the heart cannot pump blood effectively to meet the body’s needs. After an MI, the heart muscle may be weakened or damaged, leading to heart failure. This condition can develop immediately after the MI or may occur gradually over time.
SEE ALSO: What Does Nitroglycerin Do for Congestive Heart Failure
The Pathophysiology of Heart Failure After Myocardial Infarction
The transition from myocardial infarction to heart failure involves complex physiological changes. When the heart muscle is damaged, several processes can contribute to heart failure:
Loss of Myocardial Mass: An MI can cause irreversible damage to the heart muscle, leading to a loss of functional myocardial mass. This loss reduces the heart’s ability to contract effectively.
Ventricular Remodeling: After an MI, the heart undergoes structural changes known as remodeling. This process can lead to dilation of the left ventricle and changes in its shape, further impairing its function.
Neurohormonal Activation: The body responds to heart damage by activating neurohormonal systems, such as the renin-angiotensin-aldosterone system (RAAS). While these responses aim to maintain blood pressure and perfusion, they can also lead to fluid retention and increased workload on the heart, contributing to heart failure.
Increased Myocardial Oxygen Demand: The damaged heart may struggle to meet the increased oxygen demands of the body, especially during physical activity. This mismatch can lead to symptoms of heart failure.
Common Causes of Heart Failure After Myocardial Infarction
Several specific factors contribute to the development of heart failure after an MI. These causes can be categorized into immediate and long-term factors.
1. Extent of Myocardial Damage
The degree of damage to the heart muscle during an MI is a primary factor in determining whether heart failure will develop. Patients with larger infarcts or those involving critical areas of the heart, such as the left ventricle, are at a higher risk. The more extensive the damage, the greater the likelihood of heart failure.
2. Left Ventricular Dysfunction
Left ventricular dysfunction is a common consequence of myocardial infarction. When the left ventricle is unable to contract effectively, it can lead to a decrease in cardiac output. This dysfunction is often assessed using echocardiography, which can measure the ejection fraction (EF) — the percentage of blood the left ventricle pumps out with each heartbeat. An EF of less than 40% is often indicative of heart failure.
3. Ventricular Remodeling
After an MI, the heart undergoes remodeling, which can be either compensatory or maladaptive. Compensatory remodeling may initially help maintain cardiac output, but maladaptive remodeling leads to progressive heart failure. Factors contributing to maladaptive remodeling include:
Infarct Size: Larger infarcts lead to greater remodeling.
Wall Stress: Increased pressure and volume in the heart can lead to further dilation and dysfunction.
Fibrosis: Scar tissue formation in the heart can disrupt normal electrical conduction and contractility.
4. Ischemic Cardiomyopathy
Ischemic cardiomyopathy is a condition characterized by heart failure due to reduced blood flow to the heart muscle. It often results from coronary artery disease (CAD) and is a common outcome after an MI.
Patients with ischemic cardiomyopathy may experience chronic heart failure symptoms due to ongoing ischemia and damage to the heart muscle.
5. Arrhythmias
Arrhythmias, or irregular heartbeats, can occur after an MI and contribute to heart failure. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are serious arrhythmias that can lead to sudden cardiac death. Other arrhythmias, such as atrial fibrillation, can cause inefficient pumping of the heart and increase the risk of stroke, compounding heart failure symptoms.
6. Comorbid Conditions
Patients with comorbid conditions such as hypertension, diabetes, and obesity are at a higher risk of developing heart failure after an MI.
These conditions can exacerbate heart failure by increasing myocardial oxygen demand or contributing to further cardiac damage.
Hypertension: High blood pressure increases the workload on the heart and can lead to left ventricular hypertrophy, which may worsen heart failure.
Diabetes: Diabetes is associated with an increased risk of coronary artery disease and may contribute to poor outcomes after an MI.
Obesity: Excess weight can strain the heart and is linked to various cardiovascular diseases, including heart failure.
7. Inflammation and Oxidative Stress
Inflammation plays a significant role in the development of heart failure after an MI. The inflammatory response following an MI can lead to further myocardial injury and remodeling. Oxidative stress, caused by an imbalance between free radicals and antioxidants in the body, can also contribute to cardiac dysfunction.
8. Delayed Medical Intervention
Timely medical intervention after an MI is crucial in preventing heart failure. Delays in treatment, such as reperfusion therapy (e.g., angioplasty or thrombolysis), can lead to larger infarcts and increased risk of heart failure. Early identification and management of heart failure symptoms are essential for improving outcomes.
Risk Factors for Heart Failure After Myocardial Infarction
Several risk factors can increase the likelihood of developing heart failure following an MI:
Age: Older age is associated with a higher risk of heart failure due to age-related changes in the heart.
Gender: Men are generally at a higher risk of heart failure after an MI compared to women, though the risk for women increases post-menopause.
History of Heart Disease: A previous history of heart disease or heart failure increases the risk of developing heart failure after an MI.
Lifestyle Factors: Smoking, physical inactivity, and poor diet can contribute to heart disease and increase the risk of heart failure.
Prevention And Management of Heart Failure After Myocardial Infarction
Preventing heart failure after an MI involves a combination of lifestyle changes and medical management. Key strategies include:
Early Reperfusion Therapy: Timely intervention to restore blood flow to the heart is critical. This can involve medications to dissolve clots or procedures to open blocked arteries.
Medications: Patients may be prescribed medications such as ACE inhibitors, beta-blockers, and diuretics to manage heart function and reduce the risk of heart failure.
Lifestyle Modifications: Encouraging a heart-healthy lifestyle, including a balanced diet, regular exercise, and smoking cessation, can significantly reduce the risk of heart failure.
Regular Monitoring: Routine follow-up appointments with healthcare providers can help monitor heart function and detect early signs of heart failure.
Patient Education: Educating patients about the signs and symptoms of heart failure can lead to earlier intervention and better outcomes.
Conclusion
Heart failure is a common and serious complication following myocardial infarction. Understanding the causes of heart failure after an MI is crucial for prevention and management. Factors such as the extent of myocardial damage, left ventricular dysfunction, ventricular remodeling, and comorbid conditions play significant roles in the development of heart failure.
By addressing these factors through timely medical intervention, lifestyle changes, and ongoing monitoring, healthcare providers can improve outcomes for patients at risk of heart failure after myocardial infarction.