Heart failure is a complex clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s needs. It affects millions of people worldwide and is associated with high morbidity and mortality rates. The management of heart failure often requires a multifaceted approach, including lifestyle modifications, pharmacotherapy, and sometimes advanced interventions. Among the various treatment options, dopamine has emerged as a significant agent due to its unique pharmacological properties that can benefit patients with heart failure.
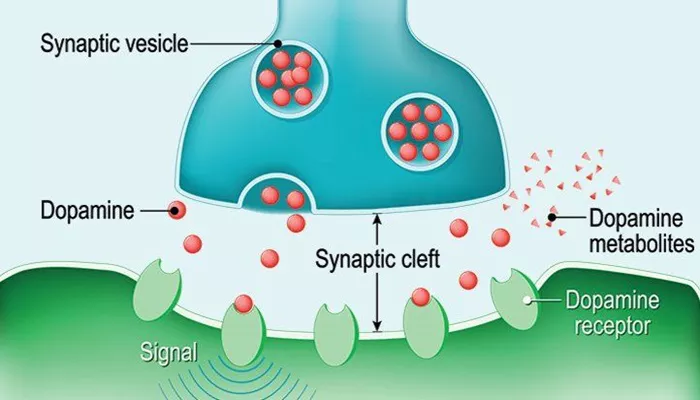
Dopamine is an endogenous catecholamine that acts as both a neurotransmitter in the central nervous system and a hormone in the peripheral circulation. It exerts its effects via multiple receptor subtypes, including dopamine receptors (D1, D2) and adrenergic receptors (α and β). The application of dopamine in heart failure is primarily based on its ability to enhance cardiac output, improve renal perfusion, and exert vasodilatory effects. Understanding the mechanisms by which dopamine operates provides insight into its therapeutic role in heart failure management.
This article delves into the reasons why dopamine is utilized in treating heart failure, highlighting its pharmacological effects, clinical applications, and potential benefits for patients suffering from this debilitating condition.
Dopamine’s Mechanisms of Action
Dopamine’s effectiveness in treating heart failure can be attributed to several key mechanisms:
1. Positive Inotropic Effect
Dopamine enhances myocardial contractility through its action on β1-adrenergic receptors. This positive inotropic effect increases the force of contraction of the heart muscle, thereby improving cardiac output.
In patients with heart failure, where diminished contractility is a hallmark, this effect can be particularly beneficial. Studies have shown that low to moderate doses of dopamine can significantly improve cardiac index without excessively increasing heart rate.
2. Renal Vasodilation
One of the critical challenges in managing heart failure is maintaining adequate renal perfusion. Dopamine induces renal vasodilation by activating D1 receptors located in the renal vasculature. This action leads to increased renal blood flow and improved glomerular filtration rate (GFR), which can help mitigate renal dysfunction commonly seen in heart failure patients. The vasodilatory effect on renal arteries also aids in reducing systemic vascular resistance, further supporting cardiac output.
SEE ALSO: How Does Heart Failure Influence Cardiac Output?
3. Natriuretic Effect
Dopamine promotes natriuresis, which is the excretion of sodium through urine. This effect helps reduce fluid overload—a common issue in heart failure that contributes to symptoms such as edema and dyspnea. By inhibiting renal tubular sodium reabsorption, dopamine assists in managing fluid balance and alleviating congestion. This natriuretic action can be particularly advantageous for patients experiencing acute decompensated heart failure.
4. Improvement of Hemodynamics
In addition to enhancing contractility and renal function, dopamine positively influences hemodynamics by increasing mean arterial pressure (MAP) while reducing left ventricular end-diastolic pressure (LVEDP). This dual effect helps optimize blood flow to vital organs while alleviating the burden on the failing heart. Improved hemodynamics can lead to better exercise tolerance and quality of life for patients.
5. Autocrine and Paracrine Effects
Dopamine is not only a systemic agent but also functions locally within the heart as an autocrine or paracrine factor. It modulates various cellular processes within cardiac myocytes, influencing calcium handling and energy metabolism. This localized action may contribute to improved myocardial function independent of systemic effects.
Clinical Applications of Dopamine in Heart Failure
Dopamine’s multifaceted actions make it a valuable tool in various clinical scenarios related to heart failure:
Acute Heart Failure Management
In acute settings, such as cardiogenic shock or severe decompensated heart failure, dopamine is often employed for its rapid effects on cardiac output and hemodynamic stability. Its ability to enhance contractility and improve renal function makes it suitable for patients requiring immediate intervention.
Bridging Therapy
Dopamine can serve as a bridging therapy for patients awaiting more definitive treatments such as mechanical circulatory support or heart transplantation. By stabilizing hemodynamics during this critical period, dopamine can help maintain organ perfusion until more permanent solutions are implemented.
Patients with Renal Dysfunction
For patients with concurrent renal impairment due to heart failure, dopamine’s renal protective effects are particularly beneficial. By improving renal blood flow and promoting natriuresis, it can help manage fluid overload while preserving kidney function.
Considerations And Limitations
While dopamine offers several advantages in treating heart failure, it is essential to recognize its limitations:
Risk of Arrhythmias
One concern with dopamine therapy is the potential for inducing arrhythmias, particularly at higher doses or in susceptible individuals. The increased myocardial oxygen demand associated with enhanced contractility may lead to adverse outcomes if not carefully monitored.
Dosing Challenges
The dosing of dopamine must be tailored to individual patient needs. Low doses primarily activate dopaminergic receptors for renal protection, while higher doses shift toward adrenergic receptor activation with increased risk of side effects.
Clinicians must balance these factors when determining appropriate dosing regimens.
Conclusion
Dopamine plays a crucial role in the management of heart failure through its positive inotropic effects, renal vasodilation, natriuretic actions, and overall improvement of hemodynamics. While it has become less favored compared to newer therapies like dobutamine in certain contexts, its utility persists—particularly in acute settings or when addressing concurrent renal dysfunction.