Ischemic heart disease (IHD) is a serious condition that affects millions of people worldwide. It occurs when the heart muscle does not receive enough blood and oxygen, primarily due to narrowed or blocked coronary arteries. This article will explore how ischemic heart disease develops, the risk factors involved, and ways to prevent it.
What is Ischemic Heart Disease?
Ischemic heart disease, also known as coronary artery disease (CAD), is characterized by reduced blood flow to the heart muscle. This reduction can lead to chest pain (angina), shortness of breath, and, in severe cases, heart attacks. The primary cause of IHD is atherosclerosis, where fatty deposits (plaque) build up in the arteries over time.
When blood flow is restricted, the heart muscle may become starved for oxygen. If this condition persists or worsens, it can result in significant damage to the heart muscle. Understanding how this disease develops is crucial for prevention and effective management.
Risk Factors for Ischemic Heart Disease
Several risk factors contribute to the development of ischemic heart disease. These can be categorized into modifiable and non-modifiable factors:
Modifiable Risk Factors
Lifestyle Choices:
Diet: A diet high in saturated fats, trans fats, and cholesterol can increase cholesterol levels and promote atherosclerosis.
Physical Inactivity: Sedentary lifestyles contribute to obesity and other risk factors like high blood pressure and diabetes.
Smoking: Tobacco use significantly increases the risk of developing IHD by damaging blood vessels and promoting plaque buildup.
Medical Conditions:
Hypertension: High blood pressure puts extra strain on the heart and arteries.
High Cholesterol Levels: Elevated LDL cholesterol levels are directly linked to increased plaque formation.
Diabetes: Both type 1 and type 2 diabetes are associated with a higher risk of IHD due to their effects on blood vessels.
Obesity: Excess body weight increases the likelihood of developing high blood pressure, diabetes, and high cholesterol.
Stress: Chronic stress may contribute to unhealthy behaviors like overeating or smoking, which can increase heart disease risk.
Non-Modifiable Risk Factors
Age: The risk of developing ischemic heart disease increases with age.
Men are generally at higher risk earlier in life than women.
Family History: A family history of heart disease can increase an individual’s risk due to genetic factors.
Gender: Men are more likely than women to develop ischemic heart disease at a younger age.
SEE ALSO: How Do Carotid Arteries Get Blocked?
Symptoms of Ischemic Heart Disease
Ischemic heart disease may not always present clear symptoms initially. However, as the condition progresses, individuals may experience:
Chest Pain (Angina): This is often described as a feeling of pressure or tightness in the chest. It may occur during physical activity or emotional stress but typically subsides with rest.
Shortness of Breath: Difficulty breathing may occur during exertion or at rest as the heart struggles to pump enough blood.
Fatigue: Unusual tiredness can be a sign that the heart is not functioning optimally.
Palpitations: An irregular heartbeat may occur due to stress on the heart muscle.
Nausea or Sweating: Some individuals may experience gastrointestinal symptoms or excessive sweating during episodes of angina.
In some cases, individuals may have “silent” ischemia, where they do not experience any noticeable symptoms despite reduced blood flow to the heart muscle.
Diagnosing Ischemic Heart Disease
If ischemic heart disease is suspected, healthcare providers will conduct several tests:
Medical History and Physical Examination: A thorough evaluation of symptoms, family history, and lifestyle factors helps assess risk levels.
Electrocardiogram (ECG): This test measures electrical activity in the heart and can reveal irregularities caused by reduced blood flow.
Stress Testing: Patients may be asked to exercise while being monitored for changes in heart function under stress conditions.
Echocardiogram: This ultrasound test provides images of the heart’s structure and function.
Coronary Angiography: This invasive procedure involves injecting dye into coronary arteries to visualize blockages using X-ray imaging.
Blood Tests: Tests may be conducted to check cholesterol levels, blood sugar levels, and markers for inflammation or cardiac damage.
Treatment Options for Ischemic Heart Disease
While ischemic heart disease cannot be cured entirely, several treatment options are available:
Lifestyle Modifications
Dietary Changes: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats helps manage cholesterol levels and overall health.
Regular Exercise: Engaging in regular physical activity strengthens the heart and improves circulation. Aim for at least 150 minutes of moderate exercise per week.
Weight Management: Maintaining a healthy weight reduces strain on the heart and lowers risks associated with obesity-related conditions.
Smoking Cessation: Quitting smoking significantly reduces cardiovascular risks and improves overall health.
Stress Management: Techniques such as meditation, yoga, or counseling can help manage stress levels effectively.
Medications
Several medications may be prescribed based on individual needs:
Antiplatelet Agents: Aspirin or other medications help prevent blood clots from forming in narrowed arteries.
Statins: These medications lower cholesterol levels and reduce plaque buildup in arteries.
Beta Blockers: These drugs help lower blood pressure and reduce strain on the heart by slowing down its rate.
ACE Inhibitors or ARBs: These medications help relax blood vessels and lower blood pressure, improving overall cardiovascular health.
Nitrates: Used to relieve chest pain by widening blood vessels and improving blood flow to the heart muscle.
Surgical Interventions
In some cases where medications are not sufficient:
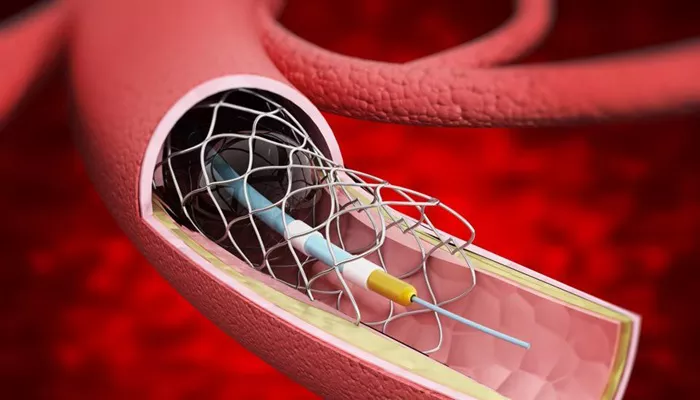
Angioplasty with Stenting: A balloon is used to open narrowed arteries while a stent is placed to keep them open permanently.
Coronary Artery Bypass Grafting (CABG): A surgical procedure that uses a vessel from another part of the body to bypass blocked coronary arteries.
Preventing Ischemic Heart Disease
Preventing ischemic heart disease involves addressing modifiable risk factors:
Regular Health Screenings: Routine check-ups help monitor blood pressure, cholesterol levels, and diabetes status early on.
Healthy Lifestyle Choices:
Eat a balanced diet low in saturated fats.
Engage in regular physical activity.
Avoid tobacco products.
Manage stress effectively.
Maintain a healthy weight through diet and exercise.
Medication Adherence: For those already diagnosed with conditions like hypertension or diabetes, taking prescribed medications consistently is vital for prevention efforts.
Conclusion
Ischemic heart disease is a significant health concern that requires awareness and proactive management. Understanding how this condition develops helps individuals make informed choices about their health. By addressing modifiable risk factors through lifestyle changes, medication adherence, and regular monitoring, it is possible to reduce the risk of developing ischemic heart disease significantly.
Related topics: