Hyperlipidemia, characterized by elevated levels of lipids in the blood, is a significant risk factor for cardiovascular diseases (CVD), including coronary artery disease, heart attacks, and strokes. It is primarily categorized into two types: hypercholesterolemia (high cholesterol) and hypertriglyceridemia (high triglycerides). Understanding how to effectively manage hyperlipidemia is crucial for reducing the incidence of CVD and improving overall health outcomes.
The management of hyperlipidemia involves a multifaceted approach that includes lifestyle modifications, dietary changes, and pharmacological interventions. This article will explore the initial steps in treating hyperlipidemia, focusing on which aspects should be prioritized to achieve optimal lipid control.
What Is Hyperlipidemia?
Hyperlipidemia can arise from genetic factors, lifestyle choices, or a combination of both. Common causes include:
Diet: High intake of saturated fats, trans fats, and cholesterol can raise lipid levels.
Obesity: Excess body weight is linked to increased levels of LDL (low-density lipoprotein) cholesterol and triglycerides.
Sedentary Lifestyle: Lack of physical activity contributes to weight gain and unhealthy lipid profiles.
Genetics: Familial hypercholesterolemia is a genetic condition that leads to high cholesterol levels.
Types of Lipids
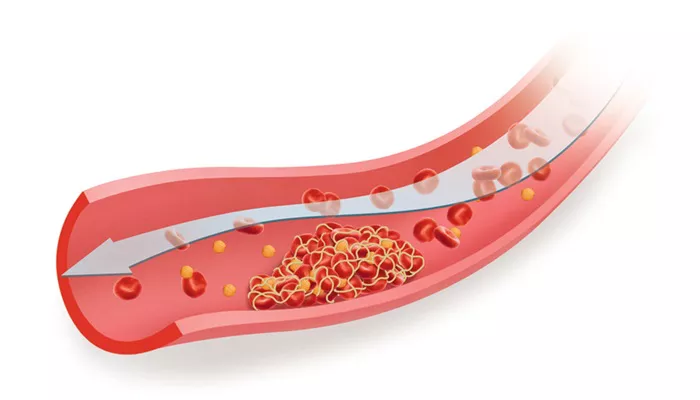
LDL Cholesterol: Often referred to as “bad” cholesterol, high levels can lead to plaque buildup in arteries.
HDL Cholesterol: Known as “good” cholesterol, it helps remove LDL cholesterol from the bloodstream.
Triglycerides: Elevated triglyceride levels are associated with an increased risk of heart disease.
Initial Treatment Strategies
Lifestyle Modifications
Before initiating pharmacotherapy, lifestyle modifications are typically recommended as the first line of treatment. These changes can significantly impact lipid levels and overall cardiovascular health.
Dietary Changes
Reduce Saturated Fats: Limiting saturated fat intake can lower LDL cholesterol levels. Foods high in saturated fats include fatty cuts of meat, full-fat dairy products, and certain oils.
Increase Fiber Intake: Soluble fiber found in oats, beans, lentils, fruits, and vegetables can reduce LDL cholesterol by binding to it in the digestive system.
Incorporate Healthy Fats: Replacing saturated fats with unsaturated fats (found in olive oil, avocados, and nuts) can improve lipid profiles.
Limit Sugar and Refined Carbs: Reducing sugar intake and avoiding processed foods can help manage triglyceride levels.
Physical Activity
Engaging in regular physical activity is essential for managing hyperlipidemia. Recommendations include:
Aerobic Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
Strength Training: Incorporate resistance training at least twice a week to improve muscle mass and metabolism.
Pharmacological Interventions
If lifestyle modifications alone do not achieve desired lipid levels after a reasonable period (typically three to six months), pharmacological interventions may be necessary.
Statins
Statins are the cornerstone of pharmacotherapy for hyperlipidemia. They work by inhibiting HMG-CoA reductase, an enzyme involved in cholesterol production in the liver. Statins have been shown to:
SEE ALSO: What Is Hypertriglyceridemia?
Reduce LDL cholesterol by 30% to 50%.
Lower the risk of cardiovascular events significantly.
Commonly prescribed statins include atorvastatin, simvastatin, and rosuvastatin. The choice of statin depends on various factors including patient tolerance, potential side effects, and specific lipid goals.
Ezetimibe
Ezetimibe is often used in conjunction with statins for patients who require further LDL reduction. It works by decreasing intestinal absorption of cholesterol.
PCSK9 Inhibitors
For patients with familial hypercholesterolemia or those who do not achieve target levels with statins alone, PCSK9 inhibitors may be considered. These medications significantly lower LDL cholesterol by enhancing the liver’s ability to remove it from the bloodstream.
Monitoring Treatment Efficacy
Regular monitoring is essential to assess the effectiveness of treatment strategies. This typically involves:
Fasting Lipid Panel: Conducted every 3-6 months after initiating treatment or adjusting medication.
Assessment of Adverse Effects: Monitoring for side effects such as muscle pain or liver enzyme abnormalities is crucial when using statins or other lipid-lowering agents.
Setting Treatment Goals
The treatment goals for hyperlipidemia depend on individual risk factors including age, family history, and existing health conditions such as diabetes or cardiovascular disease.
Risk Stratification
High-Risk Patients: Individuals with established cardiovascular disease should aim for an LDL level below 70 mg/dL.
Moderate-Risk Patients: Those with multiple risk factors may target an LDL level below 100 mg/dL.
Low-Risk Patients: A general goal for low-risk individuals may be an LDL level below 130 mg/dL.
Conclusion
Treating hyperlipidemia effectively requires a comprehensive strategy that prioritizes lifestyle modifications followed by pharmacological interventions when necessary. The initial focus should be on dietary changes and increased physical activity as these can lead to significant improvements in lipid profiles without immediate reliance on medications.
When pharmacotherapy is indicated, statins remain the first-line treatment due to their proven efficacy in reducing cardiovascular risk. Regular monitoring and individualized treatment goals are essential components of effective management strategies for hyperlipidemia.
Related topics:
- How Does Hyperlipidemia Cause Hyponatremia?
- Which Is Safer, Atorvastatin or Rosuvastatin?
- Is Bread Bad for Cholesterol?