Diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF), occurs when the heart’s left ventricle is unable to relax properly during the diastolic phase (the period when the heart fills with blood). This condition leads to increased pressure in the heart chambers and inadequate filling of the ventricle, resulting in symptoms like shortness of breath, fatigue, and fluid retention. Unlike systolic heart failure, where the heart’s pumping ability is reduced, diastolic heart failure preserves the pumping action but impairs relaxation and filling.
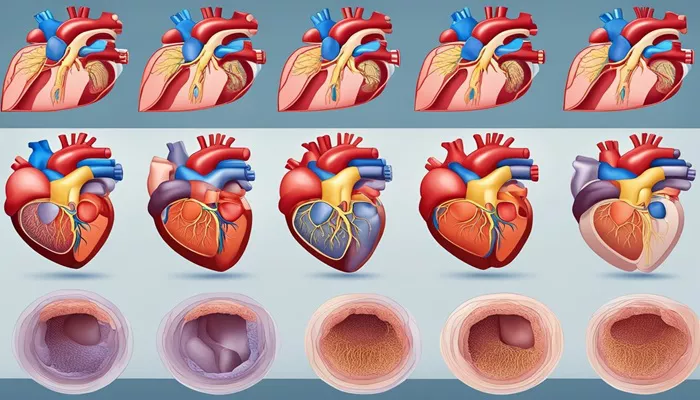
Understanding the stages of diastolic heart failure is crucial for diagnosing and managing the disease effectively. The American College of Cardiology (ACC) and the American Heart Association (AHA) classify heart failure into four progressive stages, labeled A to D. This classification helps healthcare professionals determine the severity of the disease and establish a tailored treatment plan for each patient. Let’s examine these stages in detail.
Stage A: At High Risk for Heart Failure
In Stage A, individuals are considered at high risk for developing heart failure but do not yet have structural heart disease or symptoms of heart failure. This is often referred to as the “pre-heart failure” stage. Patients in this category usually have one or more risk factors that increase the likelihood of developing diastolic heart failure in the future.
Common Risk Factors:
Hypertension (High Blood Pressure): Chronic high blood pressure can cause the heart muscle to thicken (left ventricular hypertrophy) and stiffen over time, leading to diastolic dysfunction.
Diabetes Mellitus: Diabetes is associated with metabolic abnormalities that can affect the heart’s ability to relax and fill properly.
Coronary Artery Disease (CAD): Blockages in the coronary arteries reduce blood flow to the heart muscle, leading to ischemia and potential diastolic dysfunction.
Obesity: Excessive weight puts extra strain on the heart, increasing the risk of heart failure.
Metabolic Syndrome: A combination of conditions (e.g., hypertension, obesity, high blood sugar) that heighten the risk of cardiovascular disease and heart failure.
Family History: Genetic predisposition plays a role in the development of heart failure.
Management Focus: The focus at this stage is on identifying and treating risk factors early to prevent the progression to diastolic heart failure. Lifestyle changes such as regular exercise, a balanced diet, smoking cessation, and stress management are highly recommended.
In addition, controlling blood pressure, diabetes, and cholesterol levels through medication can significantly reduce the risk.
SEE ALSO: What Does Carpal Tunnel Syndrome Have to Do with Heart Failure
Stage B: Structural Heart Disease Without Symptoms
Stage B of diastolic heart failure involves individuals who have structural heart abnormalities that can be detected through diagnostic tests but do not exhibit symptoms of heart failure. This stage is also referred to as “asymptomatic heart failure.”
Characteristics:
Left Ventricular Hypertrophy (LVH): An increase in the thickness of the heart’s walls can be seen on echocardiography. This indicates that the heart muscle is working harder than normal to pump blood, a precursor to heart failure.
Previous Heart Attack (Myocardial Infarction): Damage to the heart muscle from a previous heart attack can impair relaxation, even if the pumping ability remains normal.
Valve Disease: Conditions such as aortic stenosis (narrowing of the aortic valve) can lead to increased pressure in the heart chambers and diastolic dysfunction.
Management Focus: In Stage B, the primary goal is to slow the progression of structural changes and prevent the onset of symptoms.
This is achieved through aggressive management of underlying conditions. Medications such as ACE inhibitors, beta-blockers, and statins are commonly used to reduce the workload on the heart and manage risk factors like hypertension, high cholesterol, and CAD.
Regular monitoring of heart health through diagnostic tests (e.g., echocardiograms) is also essential.
Stage C: Symptomatic Heart Failure With Preserved Ejection Fraction
At Stage C, patients begin to show clinical symptoms of diastolic heart failure. This stage is characterized by the presence of both structural heart disease and symptoms of heart failure, such as shortness of breath, fatigue, and swelling in the legs or abdomen.
Common Symptoms:
Dyspnea (Shortness of Breath): Especially noticeable during physical activities or while lying down (orthopnea). This occurs due to increased pressure in the lungs as the heart struggles to handle blood flow efficiently.
Fatigue and Weakness: Inadequate blood flow leads to a lack of oxygen reaching muscles and tissues, causing exhaustion even during mild exertion.
Edema (Swelling): Fluid retention in the legs, ankles, and abdomen is a common sign of worsening heart function.
Palpitations: Patients may experience a rapid or irregular heartbeat as the heart tries to compensate for its reduced efficiency.
Management Focus: The treatment strategy at this stage aims to alleviate symptoms, improve quality of life, and slow disease progression. This typically involves a combination of medications, lifestyle changes, and regular follow-up with healthcare providers.
Commonly prescribed drugs include:
Diuretics: Help reduce fluid buildup and relieve symptoms of congestion and edema.
Beta-Blockers: Lower heart rate, reduce blood pressure, and improve heart relaxation.
Calcium Channel Blockers: Aid in relaxing the heart muscle, improving filling during diastole.
Aldosterone Antagonists: Reduce fluid retention and lower blood pressure.
Additionally, patients are encouraged to adopt a low-sodium diet, engage in moderate physical activity, and maintain a healthy weight.
Monitoring and managing comorbid conditions like diabetes, hypertension, and CAD remain essential to preventing further complications.
Stage D: Advanced Diastolic Heart Failure
Stage D represents the most severe form of diastolic heart failure, often called “end-stage heart failure.” Patients in this stage have significant structural heart abnormalities and experience persistent, severe symptoms despite maximal medical therapy. These symptoms may occur even at rest and are difficult to manage with standard treatments.
Symptoms:
Severe Shortness of Breath: Can be debilitating, with even minimal physical exertion causing extreme discomfort. Patients often need to sleep propped up or use supplemental oxygen.
Severe Edema: Persistent swelling in the legs, feet, abdomen, and even in the lungs (pulmonary edema), which can make breathing more difficult.
Frequent Hospitalizations: Patients in this stage may require frequent medical intervention to manage symptoms and complications.
Reduced Exercise Tolerance: Patients often find it impossible to perform even simple daily activities due to overwhelming fatigue and weakness.
Management Focus: In Stage D, the focus shifts to palliative care and improving the patient’s comfort and quality of life.
Traditional heart failure medications may no longer be sufficient, and more advanced treatments may be needed. Options include:
Mechanical Circulatory Support (MCS): Devices like left ventricular assist devices (LVADs) can help the heart pump blood more effectively.
However, these are typically reserved for patients who are candidates for heart transplantation or for temporary support.
Heart Transplantation: In suitable patients, a heart transplant may be considered as a last-resort treatment option.
Palliative Care: Symptom relief becomes a priority, and palliative care services can provide support in managing pain, breathing difficulties, and emotional well-being.
Patients and their families are often involved in making critical decisions about treatment goals and end-of-life care, focusing on minimizing discomfort and maximizing quality of life.
Conclusion
Diastolic heart failure is a complex condition that progresses through four distinct stages, each with its own set of challenges and treatment approaches. Early identification of risk factors in Stage A can prevent or delay the onset of heart failure, while effective management of structural heart disease in Stages B and C can improve outcomes and reduce symptoms. In Stage D, treatment focuses on enhancing comfort and quality of life for those with advanced disease.
Related topics: